Tuesday Poster Session
Category: Liver
P3796 - Understanding the Impact of Liver Transplantation on GI Motility: Prevalence and Risk of GERD and Gastroparesis in Transplant Recipients
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpeg.jpg)
Xiaoliang Wang, MD, PhD
Marshall University School of Medicine
Huntington, WV
Presenting Author(s)
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: The association between liver transplantation (LT) and the prevalence of gastrointestinal (GI) motility disorders such as gastroesophageal reflux disease (GERD), gastroparesis, and irritable bowel syndrome (IBS) remains under-researched, despite the frequent occurrence of related symptoms in LT patients. This study aimed to fill this knowledge gap by investigating the prevalence, risk, and correlation of these disorders in the post-LT population.
Methods: In this analysis, we utilized the Population-based National Inpatient Sample (NIS) dataset, which included data from 7,159,694 patients. Our inclusion criteria consisted of patients diagnosed with GERD (ICD-10-CM K21), gastroparesis (ICD-10-CM K31.84), and IBS (ICD-10-CM K58), regardless of their history of liver transplant (LT) (ICD-10-CM Z94.4). Patients who had undergone transplants involving other organs were excluded. We adjusted for various risk factors that could influence the prevalence of these GI motility disorders. The main focus was to determine the prevalence and odds ratio of GERD, gastroparesis, and IBS, along with concurrent GI motility disorders in LT patients. Bivariate analyses were conducted using statistical tests like the chi-squared or Fisher exact test, to assess categorical variable differences between groups.
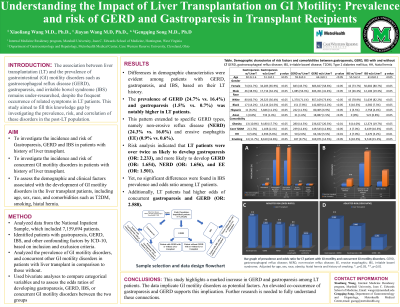
Results: Differences in demographic characteristics were evident among patients with GERD, gastroparesis, and IBS, based on their LT history. The prevalence of GERD (24.7% vs. 16.4%) and gastroparesis (1.5% vs. 0.7%) was notably higher in LT patients. This pattern extended to specific GERD types, namely non-erosive reflux disease (NERD) (24.3% vs. 16.0%) and erosive esophagitis (EE) (0.9% vs. 0.6%). Risk analysis indicated that LT patients were over twice as likely to develop gastroparesis (OR: 2.233), and more likely to develop GERD (OR: 1.654), NERD (OR: 1.656), and EE (OR: 1.501). Yet, no significant differences were found in IBS prevalence and odds ratio among LT patients. Additionally, LT patients had higher odds of concurrent gastroparesis and GERD (OR: 2.588), but no significant association was found between LT and concurrent GERD/IBS or gastroparesis/IBS.
Discussion: This study highlights a marked increase in GERD and gastroparesis among LT patients. The data implicate GI motility disorders as potential factors. An elevated co-occurrence of gastroparesis and GERD supports this implication. Further research is needed to fully understand these connections.

Disclosures:
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2. P3796 - Understanding the Impact of Liver Transplantation on GI Motility: Prevalence and Risk of GERD and Gastroparesis in Transplant Recipients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: The association between liver transplantation (LT) and the prevalence of gastrointestinal (GI) motility disorders such as gastroesophageal reflux disease (GERD), gastroparesis, and irritable bowel syndrome (IBS) remains under-researched, despite the frequent occurrence of related symptoms in LT patients. This study aimed to fill this knowledge gap by investigating the prevalence, risk, and correlation of these disorders in the post-LT population.
Methods: In this analysis, we utilized the Population-based National Inpatient Sample (NIS) dataset, which included data from 7,159,694 patients. Our inclusion criteria consisted of patients diagnosed with GERD (ICD-10-CM K21), gastroparesis (ICD-10-CM K31.84), and IBS (ICD-10-CM K58), regardless of their history of liver transplant (LT) (ICD-10-CM Z94.4). Patients who had undergone transplants involving other organs were excluded. We adjusted for various risk factors that could influence the prevalence of these GI motility disorders. The main focus was to determine the prevalence and odds ratio of GERD, gastroparesis, and IBS, along with concurrent GI motility disorders in LT patients. Bivariate analyses were conducted using statistical tests like the chi-squared or Fisher exact test, to assess categorical variable differences between groups.
Results: Differences in demographic characteristics were evident among patients with GERD, gastroparesis, and IBS, based on their LT history. The prevalence of GERD (24.7% vs. 16.4%) and gastroparesis (1.5% vs. 0.7%) was notably higher in LT patients. This pattern extended to specific GERD types, namely non-erosive reflux disease (NERD) (24.3% vs. 16.0%) and erosive esophagitis (EE) (0.9% vs. 0.6%). Risk analysis indicated that LT patients were over twice as likely to develop gastroparesis (OR: 2.233), and more likely to develop GERD (OR: 1.654), NERD (OR: 1.656), and EE (OR: 1.501). Yet, no significant differences were found in IBS prevalence and odds ratio among LT patients. Additionally, LT patients had higher odds of concurrent gastroparesis and GERD (OR: 2.588), but no significant association was found between LT and concurrent GERD/IBS or gastroparesis/IBS.
Discussion: This study highlights a marked increase in GERD and gastroparesis among LT patients. The data implicate GI motility disorders as potential factors. An elevated co-occurrence of gastroparesis and GERD supports this implication. Further research is needed to fully understand these connections.

Figure: Figure A, Demographic characterize, risk factors and comorbidities between Liver transplants with and without gastroparesis, GERD, or IBS. B, Prevalence and odds ratio of gastroparesis, GERD, IBS, and concurrent GI motility diseases in patients with history of liver transplant. C, Bar graph of prevalence and odds ratio of gastroparesis, GERD, IBS, and concurrent GI motility diseases in patients with history of Liver transplant. GERD, gastroesophageal reflux disease; NERD, non-erosive reflex disease; IBS, irritable bowel syndrome ; NERD, non-erosive reflux disease; EE, erosive esophagitis, LT, liver transplantation *, p<0.05; **, p<0.01
Disclosures:
Xiaoliang Wang indicated no relevant financial relationships.
Jiayan Wang indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2. P3796 - Understanding the Impact of Liver Transplantation on GI Motility: Prevalence and Risk of GERD and Gastroparesis in Transplant Recipients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
