Tuesday Poster Session
Category: Liver
P3797 - Unveiling the Link Between Gastrointestinal Motility Disorders and Liver Cirrhosis – A Large Scale Population-Based Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpeg.jpg)
Xiaoliang Wang, MD, PhD
Marshall University School of Medicine
Huntington, WV
Presenting Author(s)
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: While gastrointestinal (GI) symptoms are prevalent among patients with well-managed cirrhosis, they are often ascribed solely to cirrhosis, disregarding potential concurrent GI motility disorders such as gastroesophageal reflux disease (GERD), gastroparesis, and irritable bowel syndrome (IBS). This study aimed to explore the association between liver cirrhosis and these motility disorders.
Methods: We evaluated the National Inpatient Sample dataset of 7,159,694 patients, including those with GERD, gastroparesis, and IBS, with or without cirrhosis. Patients with other liver diseases were excluded. After adjusting for relevant risk factors, we primarily assessed the prevalence and odds ratios of GERD, gastroparesis, IBS, and co-existing GI motility disorders in cirrhotic patients. Categorical variable differences between groups were explored using bivariate analyses including chi-squared or Fisher's exact tests.
Results: Significant demographic variations were observed among patients with GERD or gastroparesis with or without history of cirrhosis. Cirrhosis patients exhibited notably higher prevalence of GERD (22.4% vs. 16.4%, p< 0.01) and gastroparesis (1.6% vs. 0.7%, p< 0.01) than non-cirrhotic individuals. Notably, specific GERD phenotypes like non-erosive reflux disease (NERD) (21.4% vs. 16.0%) and erosive esophagitis (EE) (1.6% vs. 0.6%) were more common among cirrhotic patients. Upon adjusting risks, cirrhosis patients were found to have 1.517-fold (95%CI: 1.441-1.597) and 1.269-fold (95%CI: 1.253-1.286) increased odds of developing gastroparesis and GERD respectively, and 1.238-fold (95%CI: 1.221-1.254) and 1.965-fold (95%CI: 1.868-2.067) elevated odds of NERD and EE respectively. Also, a higher prevalence and 1.442-fold (95%CI: 1.325-1.568) increased odds of concurrent gastroparesis and GERD were identified among cirrhotic patients (p< 0.01). However, no significant correlation was detected between cirrhosis and concurrent of GERD with IBS or gastroparesis with IBS.
Discussion: This study reveals a significant rise in GERD and gastroparesis prevalence in cirrhosis patients. The higher occurrence of concurrent gastroparesis and GERD further supports this association. Further research is needed to understand the mechanisms and implications, enabling improved management strategies for cirrhotic patients with upper GI symptoms.

Disclosures:
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2. P3797 - Unveiling the Link Between Gastrointestinal Motility Disorders and Liver Cirrhosis – A Large Scale Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Marshall University School of Medicine, Huntington, WV; 2MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: While gastrointestinal (GI) symptoms are prevalent among patients with well-managed cirrhosis, they are often ascribed solely to cirrhosis, disregarding potential concurrent GI motility disorders such as gastroesophageal reflux disease (GERD), gastroparesis, and irritable bowel syndrome (IBS). This study aimed to explore the association between liver cirrhosis and these motility disorders.
Methods: We evaluated the National Inpatient Sample dataset of 7,159,694 patients, including those with GERD, gastroparesis, and IBS, with or without cirrhosis. Patients with other liver diseases were excluded. After adjusting for relevant risk factors, we primarily assessed the prevalence and odds ratios of GERD, gastroparesis, IBS, and co-existing GI motility disorders in cirrhotic patients. Categorical variable differences between groups were explored using bivariate analyses including chi-squared or Fisher's exact tests.
Results: Significant demographic variations were observed among patients with GERD or gastroparesis with or without history of cirrhosis. Cirrhosis patients exhibited notably higher prevalence of GERD (22.4% vs. 16.4%, p< 0.01) and gastroparesis (1.6% vs. 0.7%, p< 0.01) than non-cirrhotic individuals. Notably, specific GERD phenotypes like non-erosive reflux disease (NERD) (21.4% vs. 16.0%) and erosive esophagitis (EE) (1.6% vs. 0.6%) were more common among cirrhotic patients. Upon adjusting risks, cirrhosis patients were found to have 1.517-fold (95%CI: 1.441-1.597) and 1.269-fold (95%CI: 1.253-1.286) increased odds of developing gastroparesis and GERD respectively, and 1.238-fold (95%CI: 1.221-1.254) and 1.965-fold (95%CI: 1.868-2.067) elevated odds of NERD and EE respectively. Also, a higher prevalence and 1.442-fold (95%CI: 1.325-1.568) increased odds of concurrent gastroparesis and GERD were identified among cirrhotic patients (p< 0.01). However, no significant correlation was detected between cirrhosis and concurrent of GERD with IBS or gastroparesis with IBS.
Discussion: This study reveals a significant rise in GERD and gastroparesis prevalence in cirrhosis patients. The higher occurrence of concurrent gastroparesis and GERD further supports this association. Further research is needed to understand the mechanisms and implications, enabling improved management strategies for cirrhotic patients with upper GI symptoms.

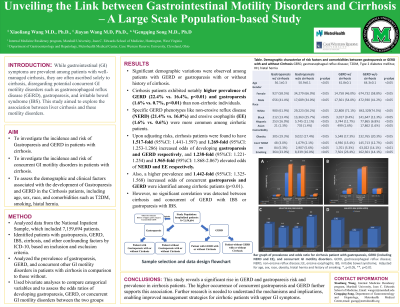
Figure: Figure A, Table of demographic characterize, risk factors and comorbidities between cirrhosis with and without gastroparesis or GERD. B, Prevalence and odds ratio of gastroparesis, GERD, and concurrent GI motility diseases in patients with cirrhosis. C, Bar graph of prevalence and odds ratio of gastroparesis, GERD and concurrent GI motility diseases in patients with cirrhosis. GERD, gastroesophageal reflux disease; NERD, non-erosive reflex disease; IBS, irritable bowel syndrome ; NERD, non-erosive reflux disease; EE, erosive esophagitis, HH, hiatal hernia. OR, odds ratio *, p<0.05; **, p<0.01
Disclosures:
Xiaoliang Wang indicated no relevant financial relationships.
Jiayan Wang indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Xiaoliang Wang, MD, PhD1, Jiayan Wang, MD, PhD1, Gengqing Song, MD2. P3797 - Unveiling the Link Between Gastrointestinal Motility Disorders and Liver Cirrhosis – A Large Scale Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
