Tuesday Poster Session
Category: Interventional Endoscopy
P3733 - Gastric Intramural Pseudocyst Causing Gastric Outlet Obstruction: Awareness and Management With a Rare Case Presentation
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ibrar Atiq, MD
United Health Services Hospital
Johnson City, NY
Presenting Author(s)
Ibrar Atiq, MD1, Adnan Khan, MD2, M'hamed Turki, MD2, Wesam Frandah, MD2, Ahmed Sherif, MD3
1United Health Services Hospital, Johnson City, NY; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Marshall University, Huntington, WV
Introduction: Intramural pseudocysts is a rare entity and first reported decades ago, heterogeneous information and limited number of cases reported in literature makes it difficult to make a firm diagnosis and appropriate treatment. Here in, we present a case of a 46 year old male to draw attention to this rare condition and help clinicians to arrive at a correct diagnosis and less aggressive treatment approach.
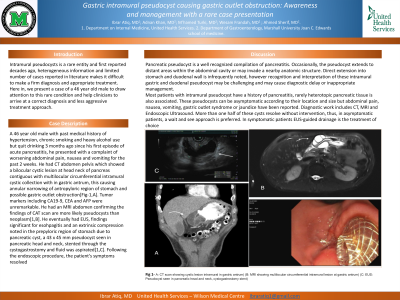
Case Description/Methods: A 46 year old male with past medical history of hypertension, chronic smoking and heavy alcohol use but quit drinking 3 months ago since his first episode of acute pancreatitis, he presented with a complaint of worsening abdominal pain, nausea and vomiting for the past 2 weeks. He had CT abdomen pelvis which showed a bilocular cystic lesion at head neck of pancreas contiguous with multilocular circumferential intramural cystic collection with in gastric antrum, this causing annular narrowing of antropyloric region of stomach and possible gastric outlet obstruction[Fig-1,A]. Tumor markers including CA19-9, CEA and AFP were unremarkable. He had an MRI abdomen confirming the findings of CAT scan are more likely pseudocysts than neoplasm[1,B]. He eventually had EUS, findings significant for esohpagitis and an extrinsic compression noted in the prepyloric region of stomach due to pancreatic cyst, a 43 x 45 mm pseudocyst seen in pancreatic head and neck, stented through the cystogastrostomy and fluid was aspirated[1,C]. Following the endoscopic procedure, the patient's symptoms resolved
Discussion: Pancreatic pseudocyst is a well recognized compilation of pancreatitis. Occasionally, the pseudocyst extends to distant areas within the abdominal cavity or may invade a nearby anatomic structure. Direct extension into stomach and duodenal wall is infrequently noted, however recognition and interpretation of these intramural gastric and duodenal pseudocyst may be challenging and may cause diagnostic delay or inappropriate management.
Most patients with intramural pseudocyst have a history of pancreatitis, rarely heterotopic pancreatic tissue is also associated. These pseudocysts can be asymptomatic according to their location and size but abdominal pain, nausea, vomiting, gastric outlet syndrome or jaundice have been reported. Diagnostic work includes CT, MRI and Endoscopic Ultrasound. More than one half of these cysts resolve without intervention, thus, in asymptomatic patients, a wait and see approach is preferred. In symptomatic patients EUS-guided drainage is the treatment of choice

Disclosures:
Ibrar Atiq, MD1, Adnan Khan, MD2, M'hamed Turki, MD2, Wesam Frandah, MD2, Ahmed Sherif, MD3. P3733 - Gastric Intramural Pseudocyst Causing Gastric Outlet Obstruction: Awareness and Management With a Rare Case Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1United Health Services Hospital, Johnson City, NY; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Marshall University, Huntington, WV
Introduction: Intramural pseudocysts is a rare entity and first reported decades ago, heterogeneous information and limited number of cases reported in literature makes it difficult to make a firm diagnosis and appropriate treatment. Here in, we present a case of a 46 year old male to draw attention to this rare condition and help clinicians to arrive at a correct diagnosis and less aggressive treatment approach.
Case Description/Methods: A 46 year old male with past medical history of hypertension, chronic smoking and heavy alcohol use but quit drinking 3 months ago since his first episode of acute pancreatitis, he presented with a complaint of worsening abdominal pain, nausea and vomiting for the past 2 weeks. He had CT abdomen pelvis which showed a bilocular cystic lesion at head neck of pancreas contiguous with multilocular circumferential intramural cystic collection with in gastric antrum, this causing annular narrowing of antropyloric region of stomach and possible gastric outlet obstruction[Fig-1,A]. Tumor markers including CA19-9, CEA and AFP were unremarkable. He had an MRI abdomen confirming the findings of CAT scan are more likely pseudocysts than neoplasm[1,B]. He eventually had EUS, findings significant for esohpagitis and an extrinsic compression noted in the prepyloric region of stomach due to pancreatic cyst, a 43 x 45 mm pseudocyst seen in pancreatic head and neck, stented through the cystogastrostomy and fluid was aspirated[1,C]. Following the endoscopic procedure, the patient's symptoms resolved
Discussion: Pancreatic pseudocyst is a well recognized compilation of pancreatitis. Occasionally, the pseudocyst extends to distant areas within the abdominal cavity or may invade a nearby anatomic structure. Direct extension into stomach and duodenal wall is infrequently noted, however recognition and interpretation of these intramural gastric and duodenal pseudocyst may be challenging and may cause diagnostic delay or inappropriate management.
Most patients with intramural pseudocyst have a history of pancreatitis, rarely heterotopic pancreatic tissue is also associated. These pseudocysts can be asymptomatic according to their location and size but abdominal pain, nausea, vomiting, gastric outlet syndrome or jaundice have been reported. Diagnostic work includes CT, MRI and Endoscopic Ultrasound. More than one half of these cysts resolve without intervention, thus, in asymptomatic patients, a wait and see approach is preferred. In symptomatic patients EUS-guided drainage is the treatment of choice

Figure: (Fig-1,A: CT scan showing cystic lesion intramural in gastric antrum) (B: MRI showing multilocular circumferential intramural lesion at gastric antrum) (C: EUS: Pseudocyst seen in pancreatic head and neck, cystogastrostomy stent)
Disclosures:
Ibrar Atiq indicated no relevant financial relationships.
Adnan Khan indicated no relevant financial relationships.
M'hamed Turki indicated no relevant financial relationships.
Wesam Frandah: Endo gastric solutions – Consultant. Olympus Medical – Consultant.
Ahmed Sherif indicated no relevant financial relationships.
Ibrar Atiq, MD1, Adnan Khan, MD2, M'hamed Turki, MD2, Wesam Frandah, MD2, Ahmed Sherif, MD3. P3733 - Gastric Intramural Pseudocyst Causing Gastric Outlet Obstruction: Awareness and Management With a Rare Case Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
