Tuesday Poster Session
Category: Interventional Endoscopy
P3745 - Intragastric Balloon Insertion Leading to Rare Complication of Acute Pancreatitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Benjamin Young, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Benjamin Young, MD1, Aaron Yazdian, MD2, Stephen Heller, MD2
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Temple University Hospital, Philadelphia, PA
Introduction: The intragastric balloon (IGB) is a non- surgical, short-term method for treatment of obesity. It functions by reducing the stomach’s capacity, thereby restricting food intake, and promoting early satiety. It is designed to remain tin the stomach for a limited period, ranging from a few months to one year, after which it is removed. Although less invasive than bariatric surgery, IGB insertion via endoscopy may lead to life threatening complications. These include gastric perforation, intestinal obstruction secondary to migration and in rare cases acute pancreatitis
Case Description/Methods: We describe a case of a 22-year-old female with past medical history significant for obesity (BMI 33) and appendectomy who presented with severe epigastric pain, nausea, and vomiting three months after intragastric balloon insertion completed in a foreign country. Serum lipase was elevated to 2624 U/L (normal 73-393 U/L) and Computerized tomography (CT) abdomen and pelvis demonstrated stranding posterior to the pancreas without evidence of fluid collection or necrosis and a large IGB in the stomach without obstruction. She was initially treated conservatively with intravenous fluids, nil per os and pain control medication. When her symptoms failed to respond after six days of management, the balloon was deflated and removed via endoscopy. She was immediately able to tolerate a diet of liquids and solids and was discharged the following day from the hospital.
Discussion: We describe a case of an intragastric balloon causing the rare complication of acute pancreatitis and the treatment of the condition with endoscopic removal. The pathogenesis of this complication has not been conclusively defined. It may be due to extrinsic compression of the body and tail of the pancreas by a dilated stomach containing the IGB, leading to mechanical trauma and inflammation. This is the first case report describing this complication in the silicone- based 350cc Silimed Gastric Balloon (Silimed Industria de Implantes Ltda Rio de Janeiro, Brazil). It serves as a reminder that patients with a history of intragastric balloon insertion and symptoms of epigastric pain, nausea and vomiting should be evaluated for pancreatitis and removal of IGB via endoscopy for resolution of their symptoms. Further research and surveillance are warranted to better understand the mechanisms and risk factors associated with this rare complication.

Disclosures:
Benjamin Young, MD1, Aaron Yazdian, MD2, Stephen Heller, MD2. P3745 - Intragastric Balloon Insertion Leading to Rare Complication of Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Temple University Hospital, Philadelphia, PA
Introduction: The intragastric balloon (IGB) is a non- surgical, short-term method for treatment of obesity. It functions by reducing the stomach’s capacity, thereby restricting food intake, and promoting early satiety. It is designed to remain tin the stomach for a limited period, ranging from a few months to one year, after which it is removed. Although less invasive than bariatric surgery, IGB insertion via endoscopy may lead to life threatening complications. These include gastric perforation, intestinal obstruction secondary to migration and in rare cases acute pancreatitis
Case Description/Methods: We describe a case of a 22-year-old female with past medical history significant for obesity (BMI 33) and appendectomy who presented with severe epigastric pain, nausea, and vomiting three months after intragastric balloon insertion completed in a foreign country. Serum lipase was elevated to 2624 U/L (normal 73-393 U/L) and Computerized tomography (CT) abdomen and pelvis demonstrated stranding posterior to the pancreas without evidence of fluid collection or necrosis and a large IGB in the stomach without obstruction. She was initially treated conservatively with intravenous fluids, nil per os and pain control medication. When her symptoms failed to respond after six days of management, the balloon was deflated and removed via endoscopy. She was immediately able to tolerate a diet of liquids and solids and was discharged the following day from the hospital.
Discussion: We describe a case of an intragastric balloon causing the rare complication of acute pancreatitis and the treatment of the condition with endoscopic removal. The pathogenesis of this complication has not been conclusively defined. It may be due to extrinsic compression of the body and tail of the pancreas by a dilated stomach containing the IGB, leading to mechanical trauma and inflammation. This is the first case report describing this complication in the silicone- based 350cc Silimed Gastric Balloon (Silimed Industria de Implantes Ltda Rio de Janeiro, Brazil). It serves as a reminder that patients with a history of intragastric balloon insertion and symptoms of epigastric pain, nausea and vomiting should be evaluated for pancreatitis and removal of IGB via endoscopy for resolution of their symptoms. Further research and surveillance are warranted to better understand the mechanisms and risk factors associated with this rare complication.

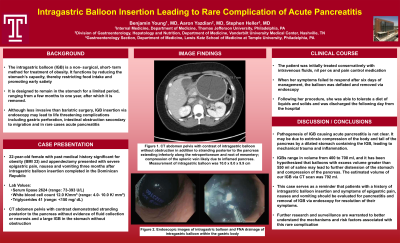
Figure: Figure 1. CT abdomen pelvis with contrast of intragastric balloon without obstruction in addition to stranding posterior to the pancreas extending inferiorly along the retroperitoneum and root of mesentery; and compression of the splenic vein likely due to the inflamed pancreas. Measurement of intragastric balloon was 10.0 x 8.0 x 9.9 cm
Disclosures:
Benjamin Young indicated no relevant financial relationships.
Aaron Yazdian indicated no relevant financial relationships.
Stephen Heller indicated no relevant financial relationships.
Benjamin Young, MD1, Aaron Yazdian, MD2, Stephen Heller, MD2. P3745 - Intragastric Balloon Insertion Leading to Rare Complication of Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
