Tuesday Poster Session
Category: Interventional Endoscopy
P3751 - From Nodules to Nodes: EUS Detects Nodal Involvement of Gangliocytic Paraganglioma
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Michael Makar, MD
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Matthew D. Still, , Graham Appelbe, DO, Michael Makar, MD, Harshit S. Khara, MD
Geisinger Medical Center, Danville, PA
Introduction: Paragangliomas are rare neuroendocrine tumors and are often grouped with pheochromocytomas, with a combined estimated annual incidence of approximately 900 cases in the United States. Many of these tumors are incidentally discovered during autopsies, indicating that a significant proportion remain undiagnosed. The limited detection rate of paragangliomas can be attributed to several factors, including lack of secretory function, small size, location within complex anatomical structures, and variable enhancement patterns on imaging.
Case Description/Methods: A 58-year-old male patient with dysphagia and persistent nausea underwent esophagogastroduodenoscopy (EGD) revealing a polypoid subepithelial lesion at the ampulla. Initial pathology findings raised concerns for a gangliocytic paraganglioma. Follow-up CT did not detect any ampullary mass or nodal involvement. The patient underwent repeat EGD with endoscopic ultrasonography (EUS) and planned endoscopic ampullectomy, pending the absence of intraductal extension or advanced local findings. During EUS, an aortocaval node was visualized and biopsied, exhibiting histological characteristics consistent with paraganglionic tissue. Subsequent PET/CT scan with 68-Ga radiotracer failed to reveal any evidence of a neuroendocrine neoplasm. The patient is scheduled for a Whipple procedure for definitive management.
Discussion: EUS has been established as a reliable modality for detecting nodal involvement in peripancreatic tumors and exhibited higher sensitivity compared to PET/CT Ga-68 and CT scan in this particular case. While the reported sensitivity of EUS for nodal involvement detection can vary and be lower than that of PET/CT Ga-68, relying solely on nuclear imaging techniques could have left this patient susceptible to further metastatic disease. This discrepancy in sensitivity may be partly attributed to the variable expression of somatostatin in neuroendocrine tumors and lymph node size. Nonetheless, the use of EUS remains justified for assessing possible nodal involvement from peripancreatic masses, even when PET/CT Ga-68 fails to detect such involvement. Our case underscores the importance of utilizing EUS for locoregional staging, as opposed to sole reliance on cross-sectional imaging, to avoid overlooking local spread and decrease the risk of metastasis.

Disclosures:
Matthew D. Still, , Graham Appelbe, DO, Michael Makar, MD, Harshit S. Khara, MD. P3751 - From Nodules to Nodes: EUS Detects Nodal Involvement of Gangliocytic Paraganglioma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Geisinger Medical Center, Danville, PA
Introduction: Paragangliomas are rare neuroendocrine tumors and are often grouped with pheochromocytomas, with a combined estimated annual incidence of approximately 900 cases in the United States. Many of these tumors are incidentally discovered during autopsies, indicating that a significant proportion remain undiagnosed. The limited detection rate of paragangliomas can be attributed to several factors, including lack of secretory function, small size, location within complex anatomical structures, and variable enhancement patterns on imaging.
Case Description/Methods: A 58-year-old male patient with dysphagia and persistent nausea underwent esophagogastroduodenoscopy (EGD) revealing a polypoid subepithelial lesion at the ampulla. Initial pathology findings raised concerns for a gangliocytic paraganglioma. Follow-up CT did not detect any ampullary mass or nodal involvement. The patient underwent repeat EGD with endoscopic ultrasonography (EUS) and planned endoscopic ampullectomy, pending the absence of intraductal extension or advanced local findings. During EUS, an aortocaval node was visualized and biopsied, exhibiting histological characteristics consistent with paraganglionic tissue. Subsequent PET/CT scan with 68-Ga radiotracer failed to reveal any evidence of a neuroendocrine neoplasm. The patient is scheduled for a Whipple procedure for definitive management.
Discussion: EUS has been established as a reliable modality for detecting nodal involvement in peripancreatic tumors and exhibited higher sensitivity compared to PET/CT Ga-68 and CT scan in this particular case. While the reported sensitivity of EUS for nodal involvement detection can vary and be lower than that of PET/CT Ga-68, relying solely on nuclear imaging techniques could have left this patient susceptible to further metastatic disease. This discrepancy in sensitivity may be partly attributed to the variable expression of somatostatin in neuroendocrine tumors and lymph node size. Nonetheless, the use of EUS remains justified for assessing possible nodal involvement from peripancreatic masses, even when PET/CT Ga-68 fails to detect such involvement. Our case underscores the importance of utilizing EUS for locoregional staging, as opposed to sole reliance on cross-sectional imaging, to avoid overlooking local spread and decrease the risk of metastasis.

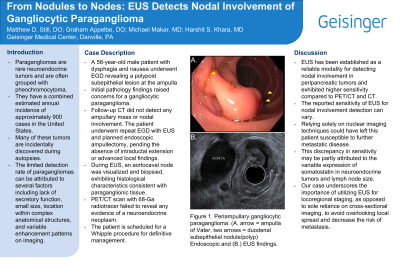
Figure: Periampullary gangliocytic paraganglioma: (A. arrow = ampulla of Vater, two arrows = duodenal subepithelial nodule/polyp) Endoscopic and (B.) EUS findings.
Disclosures:
Matthew Still indicated no relevant financial relationships.
Graham Appelbe indicated no relevant financial relationships.
Michael Makar indicated no relevant financial relationships.
Harshit Khara: Boston Scientific – Consultant, Speakers Bureau. Castle Biosciences – Consultant, Speakers Bureau. ConMed – Consultant, Speakers Bureau. Cook Medical – Consultant, Speakers Bureau. Medtronic – Consultant, Speakers Bureau. Olympus America – Consultant, Speakers Bureau. Pentax – Consultant, Speakers Bureau.
Matthew D. Still, , Graham Appelbe, DO, Michael Makar, MD, Harshit S. Khara, MD. P3751 - From Nodules to Nodes: EUS Detects Nodal Involvement of Gangliocytic Paraganglioma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
