Tuesday Poster Session
Category: Esophagus
P3290 - Impressive Finding of Tracheoesophageal Finding Due to Esophageal Malignancy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Shane Quo, DO
University of Miami at Holy Cross Hospital
Fort Lauderdale, FL
Presenting Author(s)
Shane Quo, DO1, Mary Parianos, MD2, Eduardo Villa, MD1, Hunter Carlock, MD3
1University of Miami Holy Cross Hospital, Fort Lauderdale, FL; 2University of MIami Holy Cross Hospital, Fort Lauderdale, FL; 3University of Miami, Fort Lauderdale, FL
Introduction: Esophageal cancer is increasing in frequency throughout the world raising the importance of developing effective curative and palliative treatments. However, with every treatment brings the unique possibility of unintended consequences. We present a unique case of tracheoesophageal fistula developed due to a palliative esophageal stent.
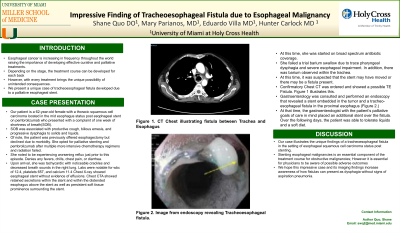
Case Description/Methods: Our patient is a 62 year old female with a thoracic squamous cell carcinoma located in the mid esophagus status post esophageal stent on pembrolizumab who presented with a complaint of one week of shortness of breath(SOB). SOB was associated with productive cough, bilious emesis, and progressive dysphagia to solids and liquids. Of note, the patient was previously offered esophagectomy but declined due to morbidity. She opted for palliative stenting and pembrolizumab after multiple more intensive chemotherapy regimens and radiation failed. She noted to be experiencing worsening reflux just prior to this episode. Denies any fevers, chills, chest pain, or diarrhea. Upon arrival, she was tachycardic with noticeable crackles and decreased breath sounds in the right lung. Labs were notable for wbc of 12.4, platelets 657, and calcium 11.4 Chest X-ray showed esophageal stent without evidence of effusions. Chest CTA showed retained secretions within the stent and within the distended esophagus above the stent as well as persistent soft tissue prominence surrounding the stent. At this time, she was started on broad spectrum antibiotic coverage. She failed a trial barium swallow due to trace pharyngeal dysphagia and severe esophageal impairment. In addition, there was barium observed within the trachea. At this time, it was suspected that the stent may have moved or there may be a fistula present. Gastroenterology was consulted and performed an endoscopy that revealed a stent embedded in the tumor and a tracheo-esophageal fistula in the proximal esophagus. At that time, the gastroenterologist with the patient’s palliative goals of care in mind placed an additional stent over the fistula. Over the following days, the patient was able to tolerate liquids and a soft diet.
Discussion: Our case illustrates the unique findings of a tracheoesophageal fistula in the setting of esophageal squamous cell carcinoma status post stenting. We hope this impressive case and its imaging findings increase awareness of how fistulas can present as dysphagia without signs of aspiration pneumonia.

Disclosures:
Shane Quo, DO1, Mary Parianos, MD2, Eduardo Villa, MD1, Hunter Carlock, MD3. P3290 - Impressive Finding of Tracheoesophageal Finding Due to Esophageal Malignancy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Miami Holy Cross Hospital, Fort Lauderdale, FL; 2University of MIami Holy Cross Hospital, Fort Lauderdale, FL; 3University of Miami, Fort Lauderdale, FL
Introduction: Esophageal cancer is increasing in frequency throughout the world raising the importance of developing effective curative and palliative treatments. However, with every treatment brings the unique possibility of unintended consequences. We present a unique case of tracheoesophageal fistula developed due to a palliative esophageal stent.
Case Description/Methods: Our patient is a 62 year old female with a thoracic squamous cell carcinoma located in the mid esophagus status post esophageal stent on pembrolizumab who presented with a complaint of one week of shortness of breath(SOB). SOB was associated with productive cough, bilious emesis, and progressive dysphagia to solids and liquids. Of note, the patient was previously offered esophagectomy but declined due to morbidity. She opted for palliative stenting and pembrolizumab after multiple more intensive chemotherapy regimens and radiation failed. She noted to be experiencing worsening reflux just prior to this episode. Denies any fevers, chills, chest pain, or diarrhea. Upon arrival, she was tachycardic with noticeable crackles and decreased breath sounds in the right lung. Labs were notable for wbc of 12.4, platelets 657, and calcium 11.4 Chest X-ray showed esophageal stent without evidence of effusions. Chest CTA showed retained secretions within the stent and within the distended esophagus above the stent as well as persistent soft tissue prominence surrounding the stent. At this time, she was started on broad spectrum antibiotic coverage. She failed a trial barium swallow due to trace pharyngeal dysphagia and severe esophageal impairment. In addition, there was barium observed within the trachea. At this time, it was suspected that the stent may have moved or there may be a fistula present. Gastroenterology was consulted and performed an endoscopy that revealed a stent embedded in the tumor and a tracheo-esophageal fistula in the proximal esophagus. At that time, the gastroenterologist with the patient’s palliative goals of care in mind placed an additional stent over the fistula. Over the following days, the patient was able to tolerate liquids and a soft diet.
Discussion: Our case illustrates the unique findings of a tracheoesophageal fistula in the setting of esophageal squamous cell carcinoma status post stenting. We hope this impressive case and its imaging findings increase awareness of how fistulas can present as dysphagia without signs of aspiration pneumonia.

Figure: Figure 1. CT chest revealing TE fistula
Disclosures:
Shane Quo indicated no relevant financial relationships.
Mary Parianos indicated no relevant financial relationships.
Eduardo Villa indicated no relevant financial relationships.
Hunter Carlock indicated no relevant financial relationships.
Shane Quo, DO1, Mary Parianos, MD2, Eduardo Villa, MD1, Hunter Carlock, MD3. P3290 - Impressive Finding of Tracheoesophageal Finding Due to Esophageal Malignancy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
