Tuesday Poster Session
Category: Biliary/Pancreas
P2902 - Coil Migration Woes
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- CE
Carter Edmunds, MD
University of Alabama at Birmingham Hospital
Birmingham, AL
Presenting Author(s)
Award: Presidential Poster Award
Carter Edmunds, MD1, Lindsay Duy, MD2, Swati Pawa, MD3
1University of Alabama at Birmingham Hospital, Birmingham, AL; 2Atrium Wake Forest Baptist Medical Center, Winston-Salem, NC; 3Atrium Health Wake Forest Baptist, Advance, NC
Introduction: Transcatheter arterial embolization (TAE) has become an increasingly valuable option for treating and preventing gastrointestinal (GI) bleeding arising from arterial aneurysms, pseudoaneurysms, and GI ulcers. Coil migration into the GI tract is an extremely rare complication of this treatment. We report one such case of coil migration into the jejunal lumen after TAE of a hepatic artery pseudoaneurysm (HAP), which was treated with endoscopy.
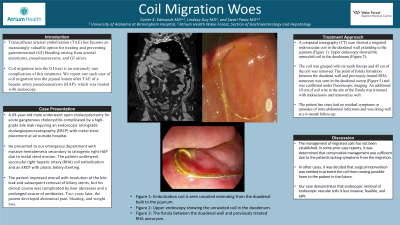
Case Description/Methods: A 69-year-old male underwent open cholecystectomy for acute gangrenous cholecystitis complicated by a high-grade bile leak requiring an endoscopic retrograde cholangiopancreatography (ERCP) with metal stent placement at an outside hospital. He presented to our emergency department with massive hematemesis secondary to iatrogenic right HAP due to metal stent erosion. The patient underwent successful right hepatic artery (RHA) coil embolization and an ERCP with plastic biliary stenting. The patient improved overall with resolution of the bile leak and subsequent removal of biliary stents, but his clinical course was complicated by liver abscesses and a prolonged course of antibiotics. Two years later, the patient developed abdominal pain, bloating, and weight loss. A computed tomography (CT) scan showed a migrated endovascular coil in the duodenal wall extending to the jejunum (Figure 1). Upper endoscopy showed the unraveled coil in the duodenum (Figure 2). The coil was grasped with rat tooth forceps and 45 cm of the coil was removed. The point of fistula formation between the duodenal wall and previously treated RHA aneurysm was seen in the duodenal sweep (Figure 3) and was confirmed under fluoroscopic imaging. An additional 10 cm of coil wire at the site of the fistula was trimmed with endoscissors and removed as well. The patient has since had no residual symptoms or episodes of intra-abdominal infections and was doing well at a 6-month follow-up.
Discussion: The management of migrated coils has not been established. In some prior case reports, it was determined that conservative management was sufficient due to the patients lacking symptoms from the migration. In other cases, it was decided that surgical intervention was needed to prevent the coil from causing possible harm to the patient in the future. Our case demonstrates that endoscopic removal of endoscopic vascular coils is less invasive, feasible, and safe.

Disclosures:
Carter Edmunds, MD1, Lindsay Duy, MD2, Swati Pawa, MD3. P2902 - Coil Migration Woes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Carter Edmunds, MD1, Lindsay Duy, MD2, Swati Pawa, MD3
1University of Alabama at Birmingham Hospital, Birmingham, AL; 2Atrium Wake Forest Baptist Medical Center, Winston-Salem, NC; 3Atrium Health Wake Forest Baptist, Advance, NC
Introduction: Transcatheter arterial embolization (TAE) has become an increasingly valuable option for treating and preventing gastrointestinal (GI) bleeding arising from arterial aneurysms, pseudoaneurysms, and GI ulcers. Coil migration into the GI tract is an extremely rare complication of this treatment. We report one such case of coil migration into the jejunal lumen after TAE of a hepatic artery pseudoaneurysm (HAP), which was treated with endoscopy.
Case Description/Methods: A 69-year-old male underwent open cholecystectomy for acute gangrenous cholecystitis complicated by a high-grade bile leak requiring an endoscopic retrograde cholangiopancreatography (ERCP) with metal stent placement at an outside hospital. He presented to our emergency department with massive hematemesis secondary to iatrogenic right HAP due to metal stent erosion. The patient underwent successful right hepatic artery (RHA) coil embolization and an ERCP with plastic biliary stenting. The patient improved overall with resolution of the bile leak and subsequent removal of biliary stents, but his clinical course was complicated by liver abscesses and a prolonged course of antibiotics. Two years later, the patient developed abdominal pain, bloating, and weight loss. A computed tomography (CT) scan showed a migrated endovascular coil in the duodenal wall extending to the jejunum (Figure 1). Upper endoscopy showed the unraveled coil in the duodenum (Figure 2). The coil was grasped with rat tooth forceps and 45 cm of the coil was removed. The point of fistula formation between the duodenal wall and previously treated RHA aneurysm was seen in the duodenal sweep (Figure 3) and was confirmed under fluoroscopic imaging. An additional 10 cm of coil wire at the site of the fistula was trimmed with endoscissors and removed as well. The patient has since had no residual symptoms or episodes of intra-abdominal infections and was doing well at a 6-month follow-up.
Discussion: The management of migrated coils has not been established. In some prior case reports, it was determined that conservative management was sufficient due to the patients lacking symptoms from the migration. In other cases, it was decided that surgical intervention was needed to prevent the coil from causing possible harm to the patient in the future. Our case demonstrates that endoscopic removal of endoscopic vascular coils is less invasive, feasible, and safe.

Figure: Figure 1: Embolization coil is seen uncoiled extending from the duodenal bulb (blue arrow) to the jejunum (green arrow). Figure 2: Upper endoscopy showing the unraveled coil in the duodenum. Figure 3: The fistula between the duodenal wall and previously treated RHA aneurysm.
Disclosures:
Carter Edmunds indicated no relevant financial relationships.
Lindsay Duy indicated no relevant financial relationships.
Swati Pawa: boston scientific corporation – Consultant.
Carter Edmunds, MD1, Lindsay Duy, MD2, Swati Pawa, MD3. P2902 - Coil Migration Woes, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

