Tuesday Poster Session
Category: Biliary/Pancreas
P2910 - A Spontaneous Gallbladder Perforation Leading to Hepatic Fistula, Gallstone Spillage, and Hepatic Abscess
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Ismail Ghafary, MD
Stony Brook University Hospital
Stony Brook, NY
Presenting Author(s)
Ismail Ghafary, MD, Sandy Ng, MD, Georgios Georgakis, MD, PhD, Lionel D'Souza, MD
Stony Brook University Hospital, Stony Brook, NY
Introduction: A spontaneous (non-traumatic) gallbladder perforation is rare. In even rarer cases, the perforation may be complicated by hepatic fistula or abscess, which is typically treated with cholecystectomy and drainage. However, there is no accepted treatment approach when a cholecystohepatic fistula leads to spilled gallstones causing hepatic abscesses refractory to drainage.
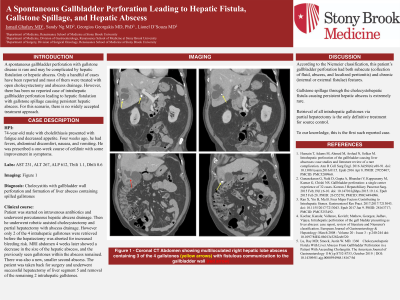
Case Description/Methods: A 74-year-old male with a past medical history of coronary artery disease, diabetes mellitus type 2, and cholelithiasis presented with fatigue and decreased appetite. Four weeks prior, he had fevers, abdominal discomfort, and vomiting and was given a course of cefdinir with some improvement. Outpatient labs showed a new transaminitis, prompting ER evaluation. On admission, the patient was hemodynamically stable. Physical exam was unremarkable. Labs were notable for elevated LFTs in a hepatocellular pattern (TBILI 1.1, DBILI 0.6, ALT 267, AST 231, and ALP 612). CT imaging showed a 7cm multiloculated right hepatic lobe abscess containing multiple calculi with fistulous communication to the gallbladder wall and a hydropic gallbladder (image 1). The clinical picture was concerning for cholecystitis with gallbladder wall perforation and subsequent formation of a liver abscess containing spilled gallstones. The patient was started on IV antibiotics and underwent percutaneous hepatic abscess drainage. He then underwent robotic assisted cholecystectomy and partial hepatectomy with abscess drainage, however only 2 of the 4 intrahepatic (spilled) calculi were able to be retrieved before the hepatectomy was aborted for increased bleeding risk. MRI Liver four weeks later showed a decrease in the size of the abscess, but the previously seen calculus within the abscess remained. There was also a new, smaller second abscess. The patient was taken back for surgery where he underwent successful hepatectomy of liver segment 5 and removal of the remaining 2 intrahepatic calculi.
Discussion: According to the Niemeier classification, our patient’s gallbladder perforation had both subacute (collection of fluid, abscess, and localized peritonitis) and chronic (internal or external fistulae) features. What makes this case extremely rare is the gallstone spillage through the cholecystohepatic fistula leading to persistent hepatic abscess. To our knowledge this is the first such reported case. It appears that retrieval of all intrahepatic gallstones via partial hepatectomy is the only definitive treatment for source control.

Disclosures:
Ismail Ghafary, MD, Sandy Ng, MD, Georgios Georgakis, MD, PhD, Lionel D'Souza, MD. P2910 - A Spontaneous Gallbladder Perforation Leading to Hepatic Fistula, Gallstone Spillage, and Hepatic Abscess, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Stony Brook University Hospital, Stony Brook, NY
Introduction: A spontaneous (non-traumatic) gallbladder perforation is rare. In even rarer cases, the perforation may be complicated by hepatic fistula or abscess, which is typically treated with cholecystectomy and drainage. However, there is no accepted treatment approach when a cholecystohepatic fistula leads to spilled gallstones causing hepatic abscesses refractory to drainage.
Case Description/Methods: A 74-year-old male with a past medical history of coronary artery disease, diabetes mellitus type 2, and cholelithiasis presented with fatigue and decreased appetite. Four weeks prior, he had fevers, abdominal discomfort, and vomiting and was given a course of cefdinir with some improvement. Outpatient labs showed a new transaminitis, prompting ER evaluation. On admission, the patient was hemodynamically stable. Physical exam was unremarkable. Labs were notable for elevated LFTs in a hepatocellular pattern (TBILI 1.1, DBILI 0.6, ALT 267, AST 231, and ALP 612). CT imaging showed a 7cm multiloculated right hepatic lobe abscess containing multiple calculi with fistulous communication to the gallbladder wall and a hydropic gallbladder (image 1). The clinical picture was concerning for cholecystitis with gallbladder wall perforation and subsequent formation of a liver abscess containing spilled gallstones. The patient was started on IV antibiotics and underwent percutaneous hepatic abscess drainage. He then underwent robotic assisted cholecystectomy and partial hepatectomy with abscess drainage, however only 2 of the 4 intrahepatic (spilled) calculi were able to be retrieved before the hepatectomy was aborted for increased bleeding risk. MRI Liver four weeks later showed a decrease in the size of the abscess, but the previously seen calculus within the abscess remained. There was also a new, smaller second abscess. The patient was taken back for surgery where he underwent successful hepatectomy of liver segment 5 and removal of the remaining 2 intrahepatic calculi.
Discussion: According to the Niemeier classification, our patient’s gallbladder perforation had both subacute (collection of fluid, abscess, and localized peritonitis) and chronic (internal or external fistulae) features. What makes this case extremely rare is the gallstone spillage through the cholecystohepatic fistula leading to persistent hepatic abscess. To our knowledge this is the first such reported case. It appears that retrieval of all intrahepatic gallstones via partial hepatectomy is the only definitive treatment for source control.

Figure: Image 1: CT Abdomen with multiloculated right hepatic lobe abscess containing 3/4 gallstones (yellow arrow) with fistulous communication to the gallbladder wall (red arrow)
Disclosures:
Ismail Ghafary indicated no relevant financial relationships.
Sandy Ng indicated no relevant financial relationships.
Georgios Georgakis indicated no relevant financial relationships.
Lionel D'Souza indicated no relevant financial relationships.
Ismail Ghafary, MD, Sandy Ng, MD, Georgios Georgakis, MD, PhD, Lionel D'Souza, MD. P2910 - A Spontaneous Gallbladder Perforation Leading to Hepatic Fistula, Gallstone Spillage, and Hepatic Abscess, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
