Tuesday Poster Session
Category: IBD
P3625 - Fecal Microbiota Transplantation and Clinical Outcomes Among Inflammatory Bowel Disease Patients: An Umbrella Review
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- SM
Sheza Malik, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Sheza Malik, MD1, Syed Arsalan Ahmed. Naqvi, 2, William Loftus, 3, Redij Renisha, MBBS2, Raseen Tariq, MBBS4, Sahil Khanna, MBBS, MS4
1Rochester General Hospital, Rochester, NY; 2Mayo Clinic, Phoenix, AZ; 3Sir Thomas Rich, Phoenix, AZ; 4Mayo Clinic, Rochester, MN
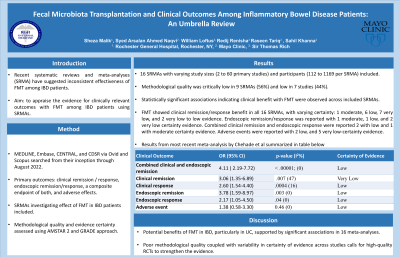
Introduction: Recent systematic reviews and meta-analyses (SRMA) have suggested inconsistent effectiveness of FMT among IBD patients. Therefore, we aimed to appraise the evidence for clinically relevant outcomes with FMT among IBD patients using published SRMAs.
Methods: To identify meta-analyses assessing effectiveness of FMT in patients with IBD, we searched MEDLINE, Embase, CENTRAL, and CDSR via Ovid and Scopus from their inception through August 2022. Our primary outcomes of interest included clinical remission/response, endoscopic remission/response, a composite endpoint of both, and adverse effects. We included SRMAs that investigated effect of FMT in IBD patients using data from both randomized controlled trials and observational studies. Methodological quality and evidence certainty was assessed using AMSTAR 2 and GRADE approach. Our own assessment was used for final adjunction if SRMAs reported their own GRADE assessment. Effect sizes were not re-estimated in this review
Results: Out of 106 citations, 16 SRMAs were included with varying study sizes (2 to 60 primary studies) and participants (112 to 1169 per SRMA). Of these, 5 SRMAs assessed FMT in patients with IBD, while 11 were focused on Ulcerative Colitis (UC). Seven SRMAs included RCTs only, and 9 SRMAs included both RCTs and observational studies. Methodological quality was critically low in 9 SRMAs (56%) and low in 7 studies (44%). Statistically significant associations indicating clinical benefit with FMT were observed across included SRMAs. FMT showed clinical remission/response benefit in all 16 SRMAs, with varying certainty: 1 moderate, 6 low, 7 very low, and 2 very low to low evidence. Endoscopic remission/response was only reported in 5 metanalyses on UC, with 1 moderate, 1 low, and 2 very low certainty evidence. Combined clinical remission and endoscopic response were reported in 3 SRMAs on UC, 2 with low and 1 with moderate certainty evidence. Adverse events were reported in 7 SRMAs, with 2 low, and 5 very low-certainty evidence. Most recent meta-analysis by Chehade et al of six RCTs (324 patients) showed clinical and endoscopic benefits in short-term treatment of active UC, with a comparable safety profile to placebo. (Table 1)
Discussion: Current evidence shows potential benefits of FMT in IBD, particularly in UC, supported by significant associations in 16 meta-analyses. However poor methodological quality coupled with variability in certainty of evidence across studies calls for high-quality RCTs to strengthen the evidence.
Disclosures:
Sheza Malik, MD1, Syed Arsalan Ahmed. Naqvi, 2, William Loftus, 3, Redij Renisha, MBBS2, Raseen Tariq, MBBS4, Sahil Khanna, MBBS, MS4. P3625 - Fecal Microbiota Transplantation and Clinical Outcomes Among Inflammatory Bowel Disease Patients: An Umbrella Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Mayo Clinic, Phoenix, AZ; 3Sir Thomas Rich, Phoenix, AZ; 4Mayo Clinic, Rochester, MN
Introduction: Recent systematic reviews and meta-analyses (SRMA) have suggested inconsistent effectiveness of FMT among IBD patients. Therefore, we aimed to appraise the evidence for clinically relevant outcomes with FMT among IBD patients using published SRMAs.
Methods: To identify meta-analyses assessing effectiveness of FMT in patients with IBD, we searched MEDLINE, Embase, CENTRAL, and CDSR via Ovid and Scopus from their inception through August 2022. Our primary outcomes of interest included clinical remission/response, endoscopic remission/response, a composite endpoint of both, and adverse effects. We included SRMAs that investigated effect of FMT in IBD patients using data from both randomized controlled trials and observational studies. Methodological quality and evidence certainty was assessed using AMSTAR 2 and GRADE approach. Our own assessment was used for final adjunction if SRMAs reported their own GRADE assessment. Effect sizes were not re-estimated in this review
Results: Out of 106 citations, 16 SRMAs were included with varying study sizes (2 to 60 primary studies) and participants (112 to 1169 per SRMA). Of these, 5 SRMAs assessed FMT in patients with IBD, while 11 were focused on Ulcerative Colitis (UC). Seven SRMAs included RCTs only, and 9 SRMAs included both RCTs and observational studies. Methodological quality was critically low in 9 SRMAs (56%) and low in 7 studies (44%). Statistically significant associations indicating clinical benefit with FMT were observed across included SRMAs. FMT showed clinical remission/response benefit in all 16 SRMAs, with varying certainty: 1 moderate, 6 low, 7 very low, and 2 very low to low evidence. Endoscopic remission/response was only reported in 5 metanalyses on UC, with 1 moderate, 1 low, and 2 very low certainty evidence. Combined clinical remission and endoscopic response were reported in 3 SRMAs on UC, 2 with low and 1 with moderate certainty evidence. Adverse events were reported in 7 SRMAs, with 2 low, and 5 very low-certainty evidence. Most recent meta-analysis by Chehade et al of six RCTs (324 patients) showed clinical and endoscopic benefits in short-term treatment of active UC, with a comparable safety profile to placebo. (Table 1)
Discussion: Current evidence shows potential benefits of FMT in IBD, particularly in UC, supported by significant associations in 16 meta-analyses. However poor methodological quality coupled with variability in certainty of evidence across studies calls for high-quality RCTs to strengthen the evidence.
Disclosures:
Sheza Malik indicated no relevant financial relationships.
Syed Naqvi indicated no relevant financial relationships.
William Loftus indicated no relevant financial relationships.
Redij Renisha indicated no relevant financial relationships.
Raseen Tariq indicated no relevant financial relationships.
Sahil Khanna: Rebiotix / Ferring, Pfizer, Vedanta – Grant/Research Support. Seres, ProBiotech, Niche, Takeda – Consultant.
Sheza Malik, MD1, Syed Arsalan Ahmed. Naqvi, 2, William Loftus, 3, Redij Renisha, MBBS2, Raseen Tariq, MBBS4, Sahil Khanna, MBBS, MS4. P3625 - Fecal Microbiota Transplantation and Clinical Outcomes Among Inflammatory Bowel Disease Patients: An Umbrella Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
