Tuesday Poster Session
Category: Liver
P4006 - A Case of Testosterone-Induced Cholestatic Liver Injury
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- RE
Rahmi Elahjji, MD
Weill Cornell Medicine
New York, New York
Presenting Author(s)
Rahmi Elahjji, MD, Suzanne Elshafey, MD, David Wan, MD
Weill Cornell Medicine, New York, NY
Introduction: Treatment with conjugated testosterone has been rarely associated with a significant cholestatic liver injury. The pathophysiology underlying this form of liver injury is poorly understood and awareness of this potential adverse effect of testosterone among patients and clinicians is limited.
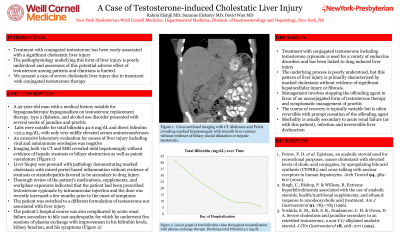
Case Description/Methods: A 42-year-old man with a medical history notable for hypogonadotropic hypogonadism on testosterone replacement therapy, type 2 diabetes mellitus, and alcohol use disorder presented with several weeks of jaundice and pruritis. Labs were notable for total bilirubin 40.6 mg/dL and direct bilirubin >22.5 mg/dL, with only very mildly elevated serum aminotransferases. An extensive laboratory evaluation for causes of liver injury including viral and autoimmune serologies was negative. Imaging via magnetic resonance cholangiopancreatography revealed mild hepatomegaly without evidence of hepatic steatosis or biliary obstruction as well as patent vasculature. Liver biopsy was pursued with pathology demonstrating marked cholestasis with mixed portal-based inflammation without evidence of steatosis or steatohepatitis favored to be secondary to drug injury. Thorough review of the patient’s medications, supplements, and workplace exposures indicated that the patient had been prescribed testosterone cypionate by intramuscular injection and the dose was recently increased a few months prior to the onset of symptoms. The patient was switched to a different formulation of testosterone not associated with liver injury. The patient’s hospital course was also complicated by acute renal failure secondary to bile cast nephropathy for which he underwent five sessions of plasma exchange with improvement in his bilirubin levels, kidney function, and his symptoms.
Discussion: Treatment with conjugated testosterone including testosterone cypionate is used for a variety of endocrine disorders and has been linked to drug induced liver injury. The underlying process is poorly understood, but this pattern of liver injury is primarily characterized by marked cholestasis without evidence of significant hepatocellular injury or fibrosis. Management involves stopping the offending agent in favor of an unconjugated form of testosterone therapy and symptomatic management of pruritis. The course of recovery is typically variable but is often reversible with prompt cessation of the offending agent. Morbidity is usually secondary to acute renal failure (as with this patient) and infection.
Disclosures:
Rahmi Elahjji, MD, Suzanne Elshafey, MD, David Wan, MD. P4006 - A Case of Testosterone-Induced Cholestatic Liver Injury, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Weill Cornell Medicine, New York, NY
Introduction: Treatment with conjugated testosterone has been rarely associated with a significant cholestatic liver injury. The pathophysiology underlying this form of liver injury is poorly understood and awareness of this potential adverse effect of testosterone among patients and clinicians is limited.
Case Description/Methods: A 42-year-old man with a medical history notable for hypogonadotropic hypogonadism on testosterone replacement therapy, type 2 diabetes mellitus, and alcohol use disorder presented with several weeks of jaundice and pruritis. Labs were notable for total bilirubin 40.6 mg/dL and direct bilirubin >22.5 mg/dL, with only very mildly elevated serum aminotransferases. An extensive laboratory evaluation for causes of liver injury including viral and autoimmune serologies was negative. Imaging via magnetic resonance cholangiopancreatography revealed mild hepatomegaly without evidence of hepatic steatosis or biliary obstruction as well as patent vasculature. Liver biopsy was pursued with pathology demonstrating marked cholestasis with mixed portal-based inflammation without evidence of steatosis or steatohepatitis favored to be secondary to drug injury. Thorough review of the patient’s medications, supplements, and workplace exposures indicated that the patient had been prescribed testosterone cypionate by intramuscular injection and the dose was recently increased a few months prior to the onset of symptoms. The patient was switched to a different formulation of testosterone not associated with liver injury. The patient’s hospital course was also complicated by acute renal failure secondary to bile cast nephropathy for which he underwent five sessions of plasma exchange with improvement in his bilirubin levels, kidney function, and his symptoms.
Discussion: Treatment with conjugated testosterone including testosterone cypionate is used for a variety of endocrine disorders and has been linked to drug induced liver injury. The underlying process is poorly understood, but this pattern of liver injury is primarily characterized by marked cholestasis without evidence of significant hepatocellular injury or fibrosis. Management involves stopping the offending agent in favor of an unconjugated form of testosterone therapy and symptomatic management of pruritis. The course of recovery is typically variable but is often reversible with prompt cessation of the offending agent. Morbidity is usually secondary to acute renal failure (as with this patient) and infection.
Disclosures:
Rahmi Elahjji indicated no relevant financial relationships.
Suzanne Elshafey indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Rahmi Elahjji, MD, Suzanne Elshafey, MD, David Wan, MD. P4006 - A Case of Testosterone-Induced Cholestatic Liver Injury, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
