Tuesday Poster Session
Category: Liver
P3895 - Diagnostic Challenge of Hepatocellular Carcinoma for Patients With Portal Vein Thrombosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Vikash Kumar, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Vikash Kumar, MD, Suut Gokturk, MD, Vijay Gayam, MD, Praneeth Bandaru, MD, Naresh kumar, MD, Arnold Forlemu, MD, MPH, Samridhi Sinha, DO, Denzil Etienne, MD
Brooklyn Hospital Center, Brooklyn, NY
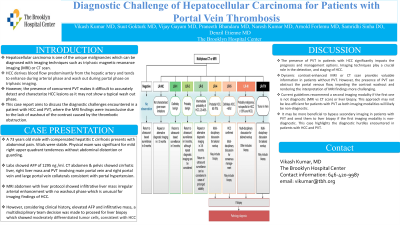
Introduction: Hepatocellular carcinoma is one of the unique malignancies which can be diagnosed with imaging techniques such as triphasic magnetic resonance imaging (MRI) or CT scan. HCC derives blood flow predominantly from the hepatic artery and tends to enhance during arterial phase and wash out during portal phase on triphasic imaging. However, the presence of concurrent PVT makes it difficult to accurately detect and characterize HCC lesions as it may not show a typical wash out phase. This case report aims to discuss the diagnostic challenges encountered in a patient with HCC and PVT, where the MRI findings were inconclusive due to the lack of washout of the contrast caused by the thrombotic obstruction.
Case Description/Methods: A 73 years old male with compensated hepatitis C cirrhosis presents with abdominal pain. Vitals were stable. Physical exam was significant for mild right upper quadrant tenderness without abdominal distention or guarding. Labs showed AFP of 1295 ng /ml. CT abdomen & pelvis showed cirrhotic liver, right liver mass and PVT involving main portal vein and right portal vein and large portal vein collaterals consistent with portal hypertension. MRI abdomen with liver protocol showed infiltrative liver mass irregular arterial enhancement with no washout phase which is unusual for imaging findings of HCC. However, considering clinical history, elevated AFP and infiltrative mass, a multidisciplinary team decision was made to proceed for liver biopsy which showed moderately differentiated tumor cells, consistent with HCC.
Discussion: The presence of PVT in patients with HCC significantly impacts the prognosis and management options. Imaging techniques play a crucial role in the detection, and staging of HCC. Dynamic contrast-enhanced MRI or CT scan provides valuable information in patients without PVT. However, the presence of PVT can obstruct the portal venous flow, impeding the contrast washout and rendering the interpretation of MRI findings more challenging. Current guidelines recommend a second imaging modality if the first one is not diagnostic (MRI vs CT scan) or liver biopsy. This approach may not be less efficient for patients with PVT as both imaging modalities will likely be non-diagnostic. It may be more beneficial to bypass secondary imaging in patients with PVT and send them to liver biopsy if the first imaging modality is non-diagnostic. This case highlights the diagnostic hurdles encountered in patients with HCC and PVT.
Disclosures:
Vikash Kumar, MD, Suut Gokturk, MD, Vijay Gayam, MD, Praneeth Bandaru, MD, Naresh kumar, MD, Arnold Forlemu, MD, MPH, Samridhi Sinha, DO, Denzil Etienne, MD. P3895 - Diagnostic Challenge of Hepatocellular Carcinoma for Patients With Portal Vein Thrombosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Brooklyn Hospital Center, Brooklyn, NY
Introduction: Hepatocellular carcinoma is one of the unique malignancies which can be diagnosed with imaging techniques such as triphasic magnetic resonance imaging (MRI) or CT scan. HCC derives blood flow predominantly from the hepatic artery and tends to enhance during arterial phase and wash out during portal phase on triphasic imaging. However, the presence of concurrent PVT makes it difficult to accurately detect and characterize HCC lesions as it may not show a typical wash out phase. This case report aims to discuss the diagnostic challenges encountered in a patient with HCC and PVT, where the MRI findings were inconclusive due to the lack of washout of the contrast caused by the thrombotic obstruction.
Case Description/Methods: A 73 years old male with compensated hepatitis C cirrhosis presents with abdominal pain. Vitals were stable. Physical exam was significant for mild right upper quadrant tenderness without abdominal distention or guarding. Labs showed AFP of 1295 ng /ml. CT abdomen & pelvis showed cirrhotic liver, right liver mass and PVT involving main portal vein and right portal vein and large portal vein collaterals consistent with portal hypertension. MRI abdomen with liver protocol showed infiltrative liver mass irregular arterial enhancement with no washout phase which is unusual for imaging findings of HCC. However, considering clinical history, elevated AFP and infiltrative mass, a multidisciplinary team decision was made to proceed for liver biopsy which showed moderately differentiated tumor cells, consistent with HCC.
Discussion: The presence of PVT in patients with HCC significantly impacts the prognosis and management options. Imaging techniques play a crucial role in the detection, and staging of HCC. Dynamic contrast-enhanced MRI or CT scan provides valuable information in patients without PVT. However, the presence of PVT can obstruct the portal venous flow, impeding the contrast washout and rendering the interpretation of MRI findings more challenging. Current guidelines recommend a second imaging modality if the first one is not diagnostic (MRI vs CT scan) or liver biopsy. This approach may not be less efficient for patients with PVT as both imaging modalities will likely be non-diagnostic. It may be more beneficial to bypass secondary imaging in patients with PVT and send them to liver biopsy if the first imaging modality is non-diagnostic. This case highlights the diagnostic hurdles encountered in patients with HCC and PVT.
Disclosures:
Vikash Kumar indicated no relevant financial relationships.
Suut Gokturk indicated no relevant financial relationships.
Vijay Gayam indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Naresh kumar indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Samridhi Sinha indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Vikash Kumar, MD, Suut Gokturk, MD, Vijay Gayam, MD, Praneeth Bandaru, MD, Naresh kumar, MD, Arnold Forlemu, MD, MPH, Samridhi Sinha, DO, Denzil Etienne, MD. P3895 - Diagnostic Challenge of Hepatocellular Carcinoma for Patients With Portal Vein Thrombosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
