Tuesday Poster Session
Category: Biliary/Pancreas
P2843 - Diagnostic Accuracy of the Urine trypsinogen-2 Dipstick Test in Early Post-ERCP Pancreatitis Prediction
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Michael Rosenheck, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Itegbemie Obaitan, MD, MPH1, Michael Rosenheck, MD1, Hisham Wehbe, MD1, Evan Fogel, MD1, Aditya Gutta, MD1, James L. Watkins, MD2, Nasir Saleem, MD1, Mark A. Gromski, MD1, Benjamin Bick, MD, MS3, Stuart Sherman, MD1, Jeffrey Easler, MD2
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University, Indianapolis, IN; 3Rockford Gastroenterology Associates, Rockford, IL
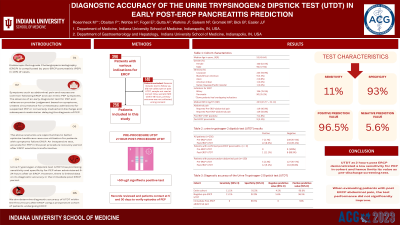
Introduction: Pancreatitis is a significant complication of Endoscopic Retrograde Cholangiopancreatoscopy (ERCP), with ~25,000 reported cases in the United States annually. An inexpensive accurate pre-discharge confirmatory test for the early diagnosis of post-ERCP pancreatitis (PEP) is lacking, and this leads to unnecessary admissions for post-procedure pain that are not PEP, as well as inadvertent discharges of patients who are subsequently readmitted with PEP. The Urine Trypsinogen-2 dipstick test (UTDT) has a high sensitivity and specificity at 24 hours post-ERCP but there is limited data on the diagnostic accuracy in the immediate post-ERCP period. Our study aim is to determine the diagnostic accuracy of this test when utilized early and explore the change in test characteristics based on the pre-procedure UTDT results and presence of post-procedure abdominal pain.
Methods: Of the 396 patients with various indications for an ERCP between July 2017 and March 2020 enrolled into a prospective study database at Indiana University Health System, 254 patients met our inclusion and exclusion criteria for this cohort study. Pre- and 2-hour post-UTDT was carried out on all patients. A cut-point of < 50ug/L delineated a negative test. Follow up data was obtained at day 5 and day 30 post-procedure. Our primary outcome was PEP. Analysis was done in STATA17.
Results: The median age of our cohort was 55 years (IQR 45-64 years), with 61.8% of our cohort being female. Immediate post-ERCP abdominal pain was reported in 50.8% of patients, with 9 (3.5%) patients in our cohort developing PEP. The Pre-ERCP UTDT positivity incidence was 2.8%. The sensitivity, specificity, positive predictive value and negative predictive value of the post-ERCP UTDT were 11.1%, 91%, 4.4% and 96.5% respectively in the entire cohort, and 11.1%, 92.9%, 5.6% and 96.5% in patients with negative pre-ERCP UTDT. In patients with post-procedure abdominal pain, these characteristics were 0%, 89.3%, 0% and 94% respectively.
Discussion: Administration of the UTDT within 2 hours of ERCP lacks adequate sensitivity to be used as a pre-discharge screening test for all patients. However, when there is a strong concern for PEP it may aid an earlier admission decision. A negative pre-ERCP UTDT only marginally improves diagnostic accuracy, so pre-procedure testing is likely not required. The presence of post-ERCP abdominal pain does not improve test accuracy. Larger cohort studies of PEP patients are needed to validate these findings.
Disclosures:
Itegbemie Obaitan, MD, MPH1, Michael Rosenheck, MD1, Hisham Wehbe, MD1, Evan Fogel, MD1, Aditya Gutta, MD1, James L. Watkins, MD2, Nasir Saleem, MD1, Mark A. Gromski, MD1, Benjamin Bick, MD, MS3, Stuart Sherman, MD1, Jeffrey Easler, MD2. P2843 - Diagnostic Accuracy of the Urine trypsinogen-2 Dipstick Test in Early Post-ERCP Pancreatitis Prediction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2Indiana University, Indianapolis, IN; 3Rockford Gastroenterology Associates, Rockford, IL
Introduction: Pancreatitis is a significant complication of Endoscopic Retrograde Cholangiopancreatoscopy (ERCP), with ~25,000 reported cases in the United States annually. An inexpensive accurate pre-discharge confirmatory test for the early diagnosis of post-ERCP pancreatitis (PEP) is lacking, and this leads to unnecessary admissions for post-procedure pain that are not PEP, as well as inadvertent discharges of patients who are subsequently readmitted with PEP. The Urine Trypsinogen-2 dipstick test (UTDT) has a high sensitivity and specificity at 24 hours post-ERCP but there is limited data on the diagnostic accuracy in the immediate post-ERCP period. Our study aim is to determine the diagnostic accuracy of this test when utilized early and explore the change in test characteristics based on the pre-procedure UTDT results and presence of post-procedure abdominal pain.
Methods: Of the 396 patients with various indications for an ERCP between July 2017 and March 2020 enrolled into a prospective study database at Indiana University Health System, 254 patients met our inclusion and exclusion criteria for this cohort study. Pre- and 2-hour post-UTDT was carried out on all patients. A cut-point of < 50ug/L delineated a negative test. Follow up data was obtained at day 5 and day 30 post-procedure. Our primary outcome was PEP. Analysis was done in STATA17.
Results: The median age of our cohort was 55 years (IQR 45-64 years), with 61.8% of our cohort being female. Immediate post-ERCP abdominal pain was reported in 50.8% of patients, with 9 (3.5%) patients in our cohort developing PEP. The Pre-ERCP UTDT positivity incidence was 2.8%. The sensitivity, specificity, positive predictive value and negative predictive value of the post-ERCP UTDT were 11.1%, 91%, 4.4% and 96.5% respectively in the entire cohort, and 11.1%, 92.9%, 5.6% and 96.5% in patients with negative pre-ERCP UTDT. In patients with post-procedure abdominal pain, these characteristics were 0%, 89.3%, 0% and 94% respectively.
Discussion: Administration of the UTDT within 2 hours of ERCP lacks adequate sensitivity to be used as a pre-discharge screening test for all patients. However, when there is a strong concern for PEP it may aid an earlier admission decision. A negative pre-ERCP UTDT only marginally improves diagnostic accuracy, so pre-procedure testing is likely not required. The presence of post-ERCP abdominal pain does not improve test accuracy. Larger cohort studies of PEP patients are needed to validate these findings.
Disclosures:
Itegbemie Obaitan indicated no relevant financial relationships.
Michael Rosenheck indicated no relevant financial relationships.
Hisham Wehbe indicated no relevant financial relationships.
Evan Fogel indicated no relevant financial relationships.
Aditya Gutta indicated no relevant financial relationships.
James Watkins indicated no relevant financial relationships.
Nasir Saleem indicated no relevant financial relationships.
Mark Gromski: Ambu – Consultant. Boston Scientific – Consultant. Cook Medical – Grant/Research Support.
Benjamin Bick indicated no relevant financial relationships.
Stuart Sherman: Boston Scientific – Consultant. Cook – Consultant. Olympus – Consultant.
Jeffrey Easler: Boston Scientific – Consultant.
Itegbemie Obaitan, MD, MPH1, Michael Rosenheck, MD1, Hisham Wehbe, MD1, Evan Fogel, MD1, Aditya Gutta, MD1, James L. Watkins, MD2, Nasir Saleem, MD1, Mark A. Gromski, MD1, Benjamin Bick, MD, MS3, Stuart Sherman, MD1, Jeffrey Easler, MD2. P2843 - Diagnostic Accuracy of the Urine trypsinogen-2 Dipstick Test in Early Post-ERCP Pancreatitis Prediction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
