Tuesday Poster Session
Category: Biliary/Pancreas
P2846 - Comparison of Local and Systemic Complications of Acute Biliary and Alcoholic Pancreatitis in the US 2016-2020: A Propensity Matched Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Waqas Rasheed, MD
Texas Tech University Health Sciences Center
Lexington, KY
Presenting Author(s)
Waqas Rasheed, MD1, Gnanashree Dharmarpandi, MD1, Muhammad Anil, MD2, Shahana ishfaque, MBBS3, Sarah Naveed. Qureshi, MBBS4, Muhammad Anees, MD1
1Texas Tech University Health Sciences Center, Amarillo, TX; 2Beaumont Hospital, Dearborn, MI; 3Punjab Medical College, Faisalabad, Pakistan, Dearborn, MI; 4CMH Multan Institute of Medical Sciences, Multan, Pakistan, Beaumont, TX
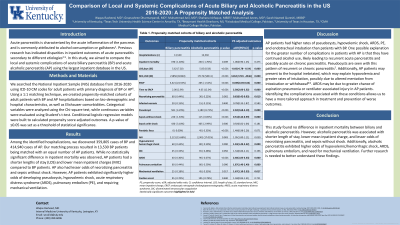
Introduction: Acute pancreatitis is characterized by the acute inflammation of the pancreas and is commonly attributed to alcohol consumption or gallstones. Previous research has indicated variations in the outcomes of AP based on its etiology. In this study, we aimed to compare the local and systemic complications of biliary pancreatitis (BP) and alcoholic pancreatitis (AP) using the largest inpatient database in the United States.
Methods: We searched the National Inpatient Sample (NIS) database from 2016-2020 using ICD-10 CM codes. Using a 1:1 matching technique, we created a propensity-matched cohort of adult patients with BP and AP hospitalizations. Categorical variables were analyzed using the Chi-square test, while continuous variables were evaluated using Student's t-test. Propensity score-adjusted outcomes were estimated through linear and logistic regression models.
Results: Among the identified hospitalizations, we discovered 359,805 cases of BP and 414,940 cases of AP. Our matching process resulted in 13,530 BP patients being matched with an equal number of AP patients. While no statistically significant difference in inpatient mortality was observed, we found that AP patients had shorter lengths of stay (LOS) and lower mean inpatient charges (MIC) compared to BP patients. AP was also associated with decreased odds of experiencing necrotizing pancreatitis and sepsis without shock. However, AP patients exhibited significantly higher odds of developing pseudocysts, hypovolemic shock, acute respiratory distress syndrome (ARDS), pulmonary embolism (PE), and requiring mechanical ventilation.
Discussion: AP patients had higher rates of pseudocysts, hypovolemic shock, ARDS, PE, and endotracheal intubation than patients with BP. One possible explanation for the greater number of complications in patients with AP is that they have continued alcohol use, likely leading to recurrent acute pancreatitis and possibly acute on chronic pancreatitis. Pseudocysts are seen with this pattern of recurrent or chronic pancreatitis. Additionally, AP patients may present to the hospital inebriated, which may explain hypovolemia and greater rates of intubation, possibly due to altered mentation from intoxication or withdrawal. ARDS may be due to greater chance of aspiration pneumonia or ventilator associated injury in AP patients. Identifying the complications associated with these conditions allows us to have a more tailored approach in treatment and prevention of worse outcomes.
Disclosures:
Waqas Rasheed, MD1, Gnanashree Dharmarpandi, MD1, Muhammad Anil, MD2, Shahana ishfaque, MBBS3, Sarah Naveed. Qureshi, MBBS4, Muhammad Anees, MD1. P2846 - Comparison of Local and Systemic Complications of Acute Biliary and Alcoholic Pancreatitis in the US 2016-2020: A Propensity Matched Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, Amarillo, TX; 2Beaumont Hospital, Dearborn, MI; 3Punjab Medical College, Faisalabad, Pakistan, Dearborn, MI; 4CMH Multan Institute of Medical Sciences, Multan, Pakistan, Beaumont, TX
Introduction: Acute pancreatitis is characterized by the acute inflammation of the pancreas and is commonly attributed to alcohol consumption or gallstones. Previous research has indicated variations in the outcomes of AP based on its etiology. In this study, we aimed to compare the local and systemic complications of biliary pancreatitis (BP) and alcoholic pancreatitis (AP) using the largest inpatient database in the United States.
Methods: We searched the National Inpatient Sample (NIS) database from 2016-2020 using ICD-10 CM codes. Using a 1:1 matching technique, we created a propensity-matched cohort of adult patients with BP and AP hospitalizations. Categorical variables were analyzed using the Chi-square test, while continuous variables were evaluated using Student's t-test. Propensity score-adjusted outcomes were estimated through linear and logistic regression models.
Results: Among the identified hospitalizations, we discovered 359,805 cases of BP and 414,940 cases of AP. Our matching process resulted in 13,530 BP patients being matched with an equal number of AP patients. While no statistically significant difference in inpatient mortality was observed, we found that AP patients had shorter lengths of stay (LOS) and lower mean inpatient charges (MIC) compared to BP patients. AP was also associated with decreased odds of experiencing necrotizing pancreatitis and sepsis without shock. However, AP patients exhibited significantly higher odds of developing pseudocysts, hypovolemic shock, acute respiratory distress syndrome (ARDS), pulmonary embolism (PE), and requiring mechanical ventilation.
Discussion: AP patients had higher rates of pseudocysts, hypovolemic shock, ARDS, PE, and endotracheal intubation than patients with BP. One possible explanation for the greater number of complications in patients with AP is that they have continued alcohol use, likely leading to recurrent acute pancreatitis and possibly acute on chronic pancreatitis. Pseudocysts are seen with this pattern of recurrent or chronic pancreatitis. Additionally, AP patients may present to the hospital inebriated, which may explain hypovolemia and greater rates of intubation, possibly due to altered mentation from intoxication or withdrawal. ARDS may be due to greater chance of aspiration pneumonia or ventilator associated injury in AP patients. Identifying the complications associated with these conditions allows us to have a more tailored approach in treatment and prevention of worse outcomes.
Disclosures:
Waqas Rasheed indicated no relevant financial relationships.
Gnanashree Dharmarpandi indicated no relevant financial relationships.
Muhammad Anil indicated no relevant financial relationships.
Shahana ishfaque indicated no relevant financial relationships.
Sarah Qureshi indicated no relevant financial relationships.
Muhammad Anees indicated no relevant financial relationships.
Waqas Rasheed, MD1, Gnanashree Dharmarpandi, MD1, Muhammad Anil, MD2, Shahana ishfaque, MBBS3, Sarah Naveed. Qureshi, MBBS4, Muhammad Anees, MD1. P2846 - Comparison of Local and Systemic Complications of Acute Biliary and Alcoholic Pancreatitis in the US 2016-2020: A Propensity Matched Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
