Tuesday Poster Session
Category: Biliary/Pancreas
P2847 - Frailty Is a Predictor for Worse Outcomes in Patients Undergoing Pancreatic Necrosectomy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- CP
Chun-Wei Pan, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Chun-Wei Pan, MD1, Bhanu Siva Mohan Pinnam, MD1, Muhammad Bilal Ibrahim, MD1, Neethi Dasu, DO2, David Truscello, DO2, Mihir Prakash Shah, MD1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Jefferson Health, New Jersey, NJ
Introduction: Acute pancreatitis is the third most common reason for gastrointestinal-related US hospital admissions, can lead to necrotizing events in up to 30% of cases. Pancreatic necrosectomy is the primary treatment, yet it's linked with substantial short- and long-term morbidity and mortality. Johns Hopkins' ACG frailty indices help identify high-risk patients for various procedures, but their use in pancreatic necrosectomy hasn't been nationally validated.
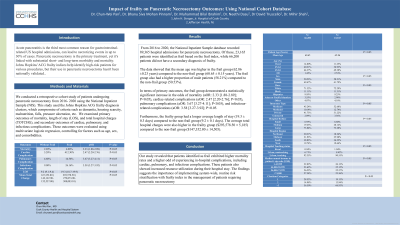
Methods: We conducted a retrospective study using National Inpatient Sample data (2016-2020) on patients who underwent pancreatic necrosectomy. Patients were classified as frail or non-frail using the Johns Hopkins ACG frailty criteria. Our analysis examined mortality, hospital stay length, total charges, and cardiac, pulmonary, and infectious complications, controlling for age, sex, and comorbidities using multivariate logistic regression.
Results: We identified 89,365 hospital admissions for pancreatic necrosectomy. Of these, 23,165 patients were identified as frail based on the frail index, while 66,200 patients did not have a secondary diagnosis of frailty.The data showed that the mean age was higher in the frail group (62.86 ±0.23 years) compared to the non-frail group (60.65 ± 0.15 years). The frail group also had a higher proportion of male patients (58.21%) compared to the non-frail group (50.53%).In terms of primary outcomes, the frail group demonstrated a statistically significant increase in the odds of mortality (aOR: 2.33 [1.88-2.89]; P< 0.05), cardiac-related complications (aOR: 2.47 [2.20-2.76]; P< 0.05), pulmonary complications (aOR: 3.67 [3.27-4.11]; P< 0.05), and infectious-related complications (aOR: 3.58 [3.27-3.92]; P< 0.05.
Furthermore, the frailty group had a longer average length of stay (19.3 ± 0.3 days) compared to the non-frail group (9.2 ± 0.1 days). The average total hospital charges were also higher in the frailty group ($293,578.50 ± 5,185) compared to the non-frail group ($147,352.80 ± 14,505).
Discussion: Our study revealed that patients identified as frail exhibited higher mortality rates and a higher odds of in-hospital events, including cardiac, pulmonary, and infectious complications. These patients also showed increased resource utilization during their hospital stay. The findings suggest the importance of implementing system-wide, routine risk stratification with frailty index in the management of patients requiring pancreatic necrosectomy.
Disclosures:
Chun-Wei Pan, MD1, Bhanu Siva Mohan Pinnam, MD1, Muhammad Bilal Ibrahim, MD1, Neethi Dasu, DO2, David Truscello, DO2, Mihir Prakash Shah, MD1. P2847 - Frailty Is a Predictor for Worse Outcomes in Patients Undergoing Pancreatic Necrosectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Jefferson Health, New Jersey, NJ
Introduction: Acute pancreatitis is the third most common reason for gastrointestinal-related US hospital admissions, can lead to necrotizing events in up to 30% of cases. Pancreatic necrosectomy is the primary treatment, yet it's linked with substantial short- and long-term morbidity and mortality. Johns Hopkins' ACG frailty indices help identify high-risk patients for various procedures, but their use in pancreatic necrosectomy hasn't been nationally validated.
Methods: We conducted a retrospective study using National Inpatient Sample data (2016-2020) on patients who underwent pancreatic necrosectomy. Patients were classified as frail or non-frail using the Johns Hopkins ACG frailty criteria. Our analysis examined mortality, hospital stay length, total charges, and cardiac, pulmonary, and infectious complications, controlling for age, sex, and comorbidities using multivariate logistic regression.
Results: We identified 89,365 hospital admissions for pancreatic necrosectomy. Of these, 23,165 patients were identified as frail based on the frail index, while 66,200 patients did not have a secondary diagnosis of frailty.The data showed that the mean age was higher in the frail group (62.86 ±0.23 years) compared to the non-frail group (60.65 ± 0.15 years). The frail group also had a higher proportion of male patients (58.21%) compared to the non-frail group (50.53%).In terms of primary outcomes, the frail group demonstrated a statistically significant increase in the odds of mortality (aOR: 2.33 [1.88-2.89]; P< 0.05), cardiac-related complications (aOR: 2.47 [2.20-2.76]; P< 0.05), pulmonary complications (aOR: 3.67 [3.27-4.11]; P< 0.05), and infectious-related complications (aOR: 3.58 [3.27-3.92]; P< 0.05.
Furthermore, the frailty group had a longer average length of stay (19.3 ± 0.3 days) compared to the non-frail group (9.2 ± 0.1 days). The average total hospital charges were also higher in the frailty group ($293,578.50 ± 5,185) compared to the non-frail group ($147,352.80 ± 14,505).
Discussion: Our study revealed that patients identified as frail exhibited higher mortality rates and a higher odds of in-hospital events, including cardiac, pulmonary, and infectious complications. These patients also showed increased resource utilization during their hospital stay. The findings suggest the importance of implementing system-wide, routine risk stratification with frailty index in the management of patients requiring pancreatic necrosectomy.
Disclosures:
Chun-Wei Pan indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Muhammad Bilal Ibrahim indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
David Truscello indicated no relevant financial relationships.
Mihir Prakash Shah indicated no relevant financial relationships.
Chun-Wei Pan, MD1, Bhanu Siva Mohan Pinnam, MD1, Muhammad Bilal Ibrahim, MD1, Neethi Dasu, DO2, David Truscello, DO2, Mihir Prakash Shah, MD1. P2847 - Frailty Is a Predictor for Worse Outcomes in Patients Undergoing Pancreatic Necrosectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
