Tuesday Poster Session
Category: Biliary/Pancreas
P2851 - Predictors of Acute Gangrenous Cholecystitis and Its Complications: A Retrospective Cohort Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kassem Barada, MD
American University of Beirut
Beirut, Beyrouth, Lebanon
Presenting Author(s)
Chantal Rizk, MD1, Dima Malak, MD1, Mohamad Ali Ibrahim, MD2, Ayman Tawil, MD1, Martine Elbejjani, PhD1, Kassem Barada, MD1, Noelle El Asmar, MD1
1American University of Beirut, Beirut, Beyrouth, Lebanon; 2American University of Beirut Medical Center, Beirut, Beyrouth, Lebanon
Introduction: Acute gangrenous cholecystitis (AGC) is a severe and serious complication of acute cholecystitis (AC). Predictors of its development and of its complications are not well established. The aims of our study were to determine factors related to AGC and its complications.
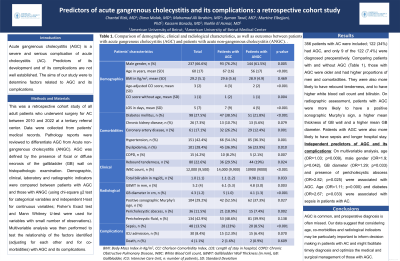
Methods: This was a retrospective cohort study of all adult patients who underwent surgery for AC between 2010 and 2022 at a tertiary referral center. Data were collected from patients’ medical records. Pathology reports were reviewed to differentiate AGC from Acute non-gangrenous cholecystitis (ANGC). AGC was defined by the presence of focal or diffuse necrosis of the gallbladder (GB) wall on histopathologic examination. Demographic, clinical, laboratory and radiographic indicators were compared between patients with AGC and those with ANGC (using chi-square χ2 test for categorical variables and independent t-test for continuous variables; Fisher’s Exact test and Mann Whitney U-test were used for variables with small number of observations). Multivariable analysis was then performed to test the relationship of the factors identified (adjusting for each other and for co-morbidities) with AGC and its complications.
Results: 356 patients with AC were included; 122 (34%) had AGC, and only 9 of the 122 (7.4%) were diagnosed preoperatively. Comparing patients with and without AGC (Table 1), those with AGC were older and had higher proportions of men and comorbidities. They were also more likely to have rebound tenderness, and to have higher white blood cell count and bilirubin. On radiographic assessment, patients with AGC were more likely to have a positive sonographic Murphy’s sign, a higher mean thickness of GB wall and a higher mean GB diameter. Patients with AGC were also more likely to have sepsis and longer hospital stay. The multivariable regression showed that age [Odds Ratio (OR)=1.03; p=0.009)], male gender (OR=1.9; p=0.042), GB diameter (OR=1.29; p=0.033) and presence of pericholecystic abscess (OR=2.82; p=0.025) were associated with AGC. Age (OR=1.11; p=0.000) and diabetes (OR=2.67; p=0.033) were associated with sepsis in patients with AC.
Discussion: AGC is common, and preoperative diagnosis is often missed. Our data suggest that considering age, co-morbidities and radiological indicators may be particularly important to inform decision making in patients with AC and might facilitate timely diagnosis and optimize the medical and surgical management of those with AGC.
Disclosures:
Chantal Rizk, MD1, Dima Malak, MD1, Mohamad Ali Ibrahim, MD2, Ayman Tawil, MD1, Martine Elbejjani, PhD1, Kassem Barada, MD1, Noelle El Asmar, MD1. P2851 - Predictors of Acute Gangrenous Cholecystitis and Its Complications: A Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1American University of Beirut, Beirut, Beyrouth, Lebanon; 2American University of Beirut Medical Center, Beirut, Beyrouth, Lebanon
Introduction: Acute gangrenous cholecystitis (AGC) is a severe and serious complication of acute cholecystitis (AC). Predictors of its development and of its complications are not well established. The aims of our study were to determine factors related to AGC and its complications.
Methods: This was a retrospective cohort study of all adult patients who underwent surgery for AC between 2010 and 2022 at a tertiary referral center. Data were collected from patients’ medical records. Pathology reports were reviewed to differentiate AGC from Acute non-gangrenous cholecystitis (ANGC). AGC was defined by the presence of focal or diffuse necrosis of the gallbladder (GB) wall on histopathologic examination. Demographic, clinical, laboratory and radiographic indicators were compared between patients with AGC and those with ANGC (using chi-square χ2 test for categorical variables and independent t-test for continuous variables; Fisher’s Exact test and Mann Whitney U-test were used for variables with small number of observations). Multivariable analysis was then performed to test the relationship of the factors identified (adjusting for each other and for co-morbidities) with AGC and its complications.
Results: 356 patients with AC were included; 122 (34%) had AGC, and only 9 of the 122 (7.4%) were diagnosed preoperatively. Comparing patients with and without AGC (Table 1), those with AGC were older and had higher proportions of men and comorbidities. They were also more likely to have rebound tenderness, and to have higher white blood cell count and bilirubin. On radiographic assessment, patients with AGC were more likely to have a positive sonographic Murphy’s sign, a higher mean thickness of GB wall and a higher mean GB diameter. Patients with AGC were also more likely to have sepsis and longer hospital stay. The multivariable regression showed that age [Odds Ratio (OR)=1.03; p=0.009)], male gender (OR=1.9; p=0.042), GB diameter (OR=1.29; p=0.033) and presence of pericholecystic abscess (OR=2.82; p=0.025) were associated with AGC. Age (OR=1.11; p=0.000) and diabetes (OR=2.67; p=0.033) were associated with sepsis in patients with AC.
Discussion: AGC is common, and preoperative diagnosis is often missed. Our data suggest that considering age, co-morbidities and radiological indicators may be particularly important to inform decision making in patients with AC and might facilitate timely diagnosis and optimize the medical and surgical management of those with AGC.
Disclosures:
Chantal Rizk indicated no relevant financial relationships.
Dima Malak indicated no relevant financial relationships.
Mohamad Ali Ibrahim indicated no relevant financial relationships.
Ayman Tawil indicated no relevant financial relationships.
Martine Elbejjani indicated no relevant financial relationships.
Kassem Barada indicated no relevant financial relationships.
Noelle El Asmar indicated no relevant financial relationships.
Chantal Rizk, MD1, Dima Malak, MD1, Mohamad Ali Ibrahim, MD2, Ayman Tawil, MD1, Martine Elbejjani, PhD1, Kassem Barada, MD1, Noelle El Asmar, MD1. P2851 - Predictors of Acute Gangrenous Cholecystitis and Its Complications: A Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
