Tuesday Poster Session
Category: Liver
P3852 - Does the Presence of In-Hospital Delirium Increase Hospital Burden and Mortality in Patients with Known Alcoholic Cirrhosis? A Population-Based Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Anmol Mittal, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Anmol Mittal, MD, Aaron Kahlam, MD, Yazan Abboud, MD, Alexander Le, MD, Kaveh Hajifathalian, MD, MPH
Rutgers New Jersey Medical School, Newark, NJ
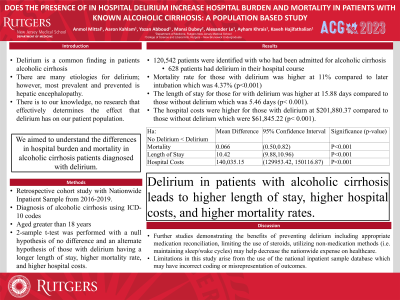
Introduction: Delirium is a common finding in patients with a history of alcoholic cirrhosis. There are many etiologies for delirium however the one most prevented is hepatic encephalopathy. There is to our knowledge, no research that effectively determines the effect that delirium has on our patient population. We aimed to understand the differences in hospital burden and mortality in alcoholic cirrhosis patients diagnosed with delirium.
Methods: A retrospective cohort study was conducted using the Nationwide Inpatient Sample from 2016-2019. All patients with a diagnosis of alcoholic cirrhosis aged greater than 18 years were included in the analysis using ICD-10 codes. A 2-sample t-test was performed with a null hypothesis of no difference and an alternate hypothesis of those with delirium having a longer length of stay, higher mortality rate, and higher hospital costs.
Results: A total of 120,542 patients were identified with who had been admitted for alcoholic cirrhosis of whom, 628 patients had delirium in their hospital course. The mortality rate for those with delirium was higher at 11% compared to later intubation which was 4.37% (p< 0.001). The length of stay for those with delirium was higher at 15.88 days compared to those without delirium which was 5.46 days (p< 0.001). The hospital costs were higher for those with delirium at $201,880.37 compared to those without delirium which were $61,845.22 (p< 0.001).
Discussion: When comparing the hospital utilization and burden including length of stay, hospital costs, and mortality rates it is demonstrated that patients in our sample with delirium had worse morbidity and mortality. Further studies demonstrating the benefits of preventing delirium including appropriate medication reconciliation, limiting the use of steroids, utilizing non-medication methods (i.e. maintaining sleep/wake cycles) may help decrease the nationwide expense on healthcare.

Disclosures:
Anmol Mittal, MD, Aaron Kahlam, MD, Yazan Abboud, MD, Alexander Le, MD, Kaveh Hajifathalian, MD, MPH. P3852 - Does the Presence of In-Hospital Delirium Increase Hospital Burden and Mortality in Patients with Known Alcoholic Cirrhosis? A Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Rutgers New Jersey Medical School, Newark, NJ
Introduction: Delirium is a common finding in patients with a history of alcoholic cirrhosis. There are many etiologies for delirium however the one most prevented is hepatic encephalopathy. There is to our knowledge, no research that effectively determines the effect that delirium has on our patient population. We aimed to understand the differences in hospital burden and mortality in alcoholic cirrhosis patients diagnosed with delirium.
Methods: A retrospective cohort study was conducted using the Nationwide Inpatient Sample from 2016-2019. All patients with a diagnosis of alcoholic cirrhosis aged greater than 18 years were included in the analysis using ICD-10 codes. A 2-sample t-test was performed with a null hypothesis of no difference and an alternate hypothesis of those with delirium having a longer length of stay, higher mortality rate, and higher hospital costs.
Results: A total of 120,542 patients were identified with who had been admitted for alcoholic cirrhosis of whom, 628 patients had delirium in their hospital course. The mortality rate for those with delirium was higher at 11% compared to later intubation which was 4.37% (p< 0.001). The length of stay for those with delirium was higher at 15.88 days compared to those without delirium which was 5.46 days (p< 0.001). The hospital costs were higher for those with delirium at $201,880.37 compared to those without delirium which were $61,845.22 (p< 0.001).
Discussion: When comparing the hospital utilization and burden including length of stay, hospital costs, and mortality rates it is demonstrated that patients in our sample with delirium had worse morbidity and mortality. Further studies demonstrating the benefits of preventing delirium including appropriate medication reconciliation, limiting the use of steroids, utilizing non-medication methods (i.e. maintaining sleep/wake cycles) may help decrease the nationwide expense on healthcare.

Figure: Table 1. Mean differences of mortality, length of stay, and hospital costs between patients with and without delirium.
Disclosures:
Anmol Mittal indicated no relevant financial relationships.
Aaron Kahlam indicated no relevant financial relationships.
Yazan Abboud indicated no relevant financial relationships.
Alexander Le indicated no relevant financial relationships.
Kaveh Hajifathalian indicated no relevant financial relationships.
Anmol Mittal, MD, Aaron Kahlam, MD, Yazan Abboud, MD, Alexander Le, MD, Kaveh Hajifathalian, MD, MPH. P3852 - Does the Presence of In-Hospital Delirium Increase Hospital Burden and Mortality in Patients with Known Alcoholic Cirrhosis? A Population-Based Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
