Tuesday Poster Session
Category: Biliary/Pancreas
P2852 - Association Between Neighborhood Opportunity and Guideline Concordant Hepatocellular Carcinoma Surveillance
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Joanna Jiang, MD
The Ohio State Wexner Medical Center
Columbus, OH
Presenting Author(s)
Erin Bouquet, MD1, Joanna Jiang, MD1, Bipul Gnyawali, BS, MD2, Dayssy A.. Diaz, MD, MS3, Lanla F. Conteh, MD, MBA, MPH2, Mohamed I. Elsaid, PhD, MPH4, Lindsay A. Sobotka, DO1
1The Ohio State Wexner Medical Center, Columbus, OH; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3Center for Biostatistics, The Ohio State University Wexner Medical Center, Columbus, OH; 4The Ohio State University, Columbus, OH
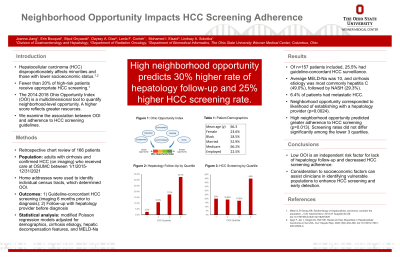
Introduction: Social disparities are prevalent in cancer screening adherence. The 2014-2018 Ohio Opportunity Index (OOI) is a multidimensional tool to quantify neighborhood-level opportunity. A high score – derived from variables including local transportation, education, employment, health, housing, crime, and environment – reflects greater resources while a low score conveys increased risk due to diminished resources. The association between OOI and HCC screening was studied.
Methods: This observational retrospective study evaluated patients with cirrhosis and HCC who received care at The Ohio State University Wexner Medical Center between 1/1/2015 and 12/31/2021. Modified Poisson regression models with robust variance adjusted for demographics, cirrhosis etiology, hepatic decompensation features, and the Model for End-Stage Liver Disease-Sodium (MELD-Na) score to examine the associations, on the prevalence ratio (aPR) scale, between guideline-concordant HCC screening (defined as completion of abdominal imaging every 6 months) and high neighborhood opportunity status. A high opportunity was defined as scores greater than the cohort’s third quartile.
Results: The study included 157 patients with cirrhosis and HCC. Patient demographics included an average age of 66.3 years, 23.6% female, 18.5% Caucasian, 52.9% were married, 66.2% had Medicare, and 67.5% were unemployed or retired. This most common etiology of cirrhosis was viral hepatitis C and alcohol and the average MELD-Na score was 10. Patients with high OOI were more likely to follow up with a hepatology provider before diagnosis of HCC than those with low OOI (32.5% vs. 10.3%, p=0.0009). Only 25.5% of patients with cirrhosis had guideline-concordant HCC screening. The prevalence of guideline-concordant HCC screening was significantly higher amongst patients with high vs. low OOI (45.0% vs. 18.8%, p=0.0001), prevalence difference of 26.2% (95% CI: 9.8% to 42.6%). The adjusted prevalence ratio of guideline-concordant HCC screening was significantly higher in patients with high vs low OOI (aPR 2.25,95% CI: 1.26 to 3.99).
Discussion: There is a significant difference in guideline-concordant HCC screening between patients with high vs. low OOI, even when controlled for clinical and demographic variables. Consideration to socioeconomic contextual factors can assist clinicians, particularly non-hepatology providers, in identifying vulnerable populations to enhance HCC screening and early detection.
Disclosures:
Erin Bouquet, MD1, Joanna Jiang, MD1, Bipul Gnyawali, BS, MD2, Dayssy A.. Diaz, MD, MS3, Lanla F. Conteh, MD, MBA, MPH2, Mohamed I. Elsaid, PhD, MPH4, Lindsay A. Sobotka, DO1. P2852 - Association Between Neighborhood Opportunity and Guideline Concordant Hepatocellular Carcinoma Surveillance, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1The Ohio State Wexner Medical Center, Columbus, OH; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3Center for Biostatistics, The Ohio State University Wexner Medical Center, Columbus, OH; 4The Ohio State University, Columbus, OH
Introduction: Social disparities are prevalent in cancer screening adherence. The 2014-2018 Ohio Opportunity Index (OOI) is a multidimensional tool to quantify neighborhood-level opportunity. A high score – derived from variables including local transportation, education, employment, health, housing, crime, and environment – reflects greater resources while a low score conveys increased risk due to diminished resources. The association between OOI and HCC screening was studied.
Methods: This observational retrospective study evaluated patients with cirrhosis and HCC who received care at The Ohio State University Wexner Medical Center between 1/1/2015 and 12/31/2021. Modified Poisson regression models with robust variance adjusted for demographics, cirrhosis etiology, hepatic decompensation features, and the Model for End-Stage Liver Disease-Sodium (MELD-Na) score to examine the associations, on the prevalence ratio (aPR) scale, between guideline-concordant HCC screening (defined as completion of abdominal imaging every 6 months) and high neighborhood opportunity status. A high opportunity was defined as scores greater than the cohort’s third quartile.
Results: The study included 157 patients with cirrhosis and HCC. Patient demographics included an average age of 66.3 years, 23.6% female, 18.5% Caucasian, 52.9% were married, 66.2% had Medicare, and 67.5% were unemployed or retired. This most common etiology of cirrhosis was viral hepatitis C and alcohol and the average MELD-Na score was 10. Patients with high OOI were more likely to follow up with a hepatology provider before diagnosis of HCC than those with low OOI (32.5% vs. 10.3%, p=0.0009). Only 25.5% of patients with cirrhosis had guideline-concordant HCC screening. The prevalence of guideline-concordant HCC screening was significantly higher amongst patients with high vs. low OOI (45.0% vs. 18.8%, p=0.0001), prevalence difference of 26.2% (95% CI: 9.8% to 42.6%). The adjusted prevalence ratio of guideline-concordant HCC screening was significantly higher in patients with high vs low OOI (aPR 2.25,95% CI: 1.26 to 3.99).
Discussion: There is a significant difference in guideline-concordant HCC screening between patients with high vs. low OOI, even when controlled for clinical and demographic variables. Consideration to socioeconomic contextual factors can assist clinicians, particularly non-hepatology providers, in identifying vulnerable populations to enhance HCC screening and early detection.
Disclosures:
Erin Bouquet indicated no relevant financial relationships.
Joanna Jiang indicated no relevant financial relationships.
Bipul Gnyawali indicated no relevant financial relationships.
Dayssy Diaz indicated no relevant financial relationships.
Lanla Conteh indicated no relevant financial relationships.
Mohamed Elsaid indicated no relevant financial relationships.
Lindsay Sobotka indicated no relevant financial relationships.
Erin Bouquet, MD1, Joanna Jiang, MD1, Bipul Gnyawali, BS, MD2, Dayssy A.. Diaz, MD, MS3, Lanla F. Conteh, MD, MBA, MPH2, Mohamed I. Elsaid, PhD, MPH4, Lindsay A. Sobotka, DO1. P2852 - Association Between Neighborhood Opportunity and Guideline Concordant Hepatocellular Carcinoma Surveillance, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
