Tuesday Poster Session
Category: Liver
P3853 - Disease Recurrence After Liver Transplantation for NASH Is Higher Than Alcohol-Associated Cirrhosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Smruti Rath, MD
Mount Sinai Hospital
New York, NY
Presenting Author(s)
Smruti Rath, MD1, Ishaan Dharia, MD2, Gene Im, MD3
1Mount Sinai Hospital, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Recanati/Miller Transplantation Institute, Icahn School of Medicine at Mount Sinai, New York, NY
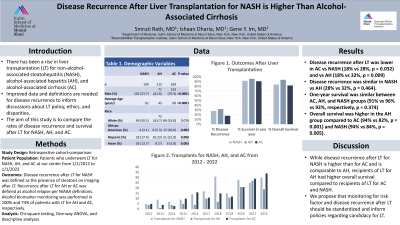
Introduction: Disease recurrence after liver transplantation (LT) is varied and etiology specific. Given the rise of LT for the steatotic liver diseases, non-alcohol-associated steatohepatitis (NASH), alcohol-associated cirrhosis (AC) and alcohol-associated hepatitis (AH), improved data and definitions are needed for disease recurrence to inform discussions about LT policy, ethics and disparities. The aim of this study is to determine and compare the outcomes of disease recurrence and survival in LT for NASH, AC, and AH.
Methods: Using a prospectively maintained database, we performed a retrospective cohort-comparison study of patients who underwent LT for NASH and alcohol-associated liver disease (ALD) at our center from 1/1/2012 to 1/1/2023. We gathered and analyzed data regarding patient demographics, radiologic imaging, and alcohol consumption after LT from alcohol biomarker monitoring (urine ethyl glucuronide and/or phosphatidylethanol), and patient survival. Disease recurrence after LT for NASH was defined as the presence of steatosis on imaging after LT. Recurrence after LT for ALD was defined as alcohol relapse per NIAAA definitions.
Results: Over the 11-year study period, 190 LT for NASH, 160 LT for AC, and 113 LT for AH were performed at our center. The group of recipients of LT for AC had a lower proportion of women compared to the group for AH (23% vs 38%, p = 0.008) and NASH (23% vs 46%, p = 0.00001) with no significant difference between the proportion of women in groups with LT for AH and NASH (38% vs 46%, p = 0.188). Recipients of LT for AH were younger than recipients of LT for AC and NASH (median [IQR]: 43 years [36-51] vs 60 years [52.5-65] vs 62.5 years [56-67]). Alcohol biomarker monitoring was performed in 100% and 74% of LT for AH and AC recipients, respectively. Notably, disease recurrence after LT was lower in AC vs NASH (18% vs 28%, p = 0.032) and vs AH (18% vs 32%, p = 0.009); however, recurrence was similar in NASH vs AH (28% vs 32%, p = 0.464). While one-year survival was similar between AC, AH, and NASH groups (91% vs 96% vs 92%, respectively, p = 0.374), recipients of LT for AH had higher overall survival compared to AC (94% vs 82%, p = 0.001) and NASH (94% vs 84%, p = 0.005).
Discussion: While disease recurrence after LT for NASH is higher than AC, but similar to AH, recipients of LT for AH had higher overall survival compared to recipients of LT for AC and NASH.

Disclosures:
Smruti Rath, MD1, Ishaan Dharia, MD2, Gene Im, MD3. P3853 - Disease Recurrence After Liver Transplantation for NASH Is Higher Than Alcohol-Associated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai Hospital, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Recanati/Miller Transplantation Institute, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Disease recurrence after liver transplantation (LT) is varied and etiology specific. Given the rise of LT for the steatotic liver diseases, non-alcohol-associated steatohepatitis (NASH), alcohol-associated cirrhosis (AC) and alcohol-associated hepatitis (AH), improved data and definitions are needed for disease recurrence to inform discussions about LT policy, ethics and disparities. The aim of this study is to determine and compare the outcomes of disease recurrence and survival in LT for NASH, AC, and AH.
Methods: Using a prospectively maintained database, we performed a retrospective cohort-comparison study of patients who underwent LT for NASH and alcohol-associated liver disease (ALD) at our center from 1/1/2012 to 1/1/2023. We gathered and analyzed data regarding patient demographics, radiologic imaging, and alcohol consumption after LT from alcohol biomarker monitoring (urine ethyl glucuronide and/or phosphatidylethanol), and patient survival. Disease recurrence after LT for NASH was defined as the presence of steatosis on imaging after LT. Recurrence after LT for ALD was defined as alcohol relapse per NIAAA definitions.
Results: Over the 11-year study period, 190 LT for NASH, 160 LT for AC, and 113 LT for AH were performed at our center. The group of recipients of LT for AC had a lower proportion of women compared to the group for AH (23% vs 38%, p = 0.008) and NASH (23% vs 46%, p = 0.00001) with no significant difference between the proportion of women in groups with LT for AH and NASH (38% vs 46%, p = 0.188). Recipients of LT for AH were younger than recipients of LT for AC and NASH (median [IQR]: 43 years [36-51] vs 60 years [52.5-65] vs 62.5 years [56-67]). Alcohol biomarker monitoring was performed in 100% and 74% of LT for AH and AC recipients, respectively. Notably, disease recurrence after LT was lower in AC vs NASH (18% vs 28%, p = 0.032) and vs AH (18% vs 32%, p = 0.009); however, recurrence was similar in NASH vs AH (28% vs 32%, p = 0.464). While one-year survival was similar between AC, AH, and NASH groups (91% vs 96% vs 92%, respectively, p = 0.374), recipients of LT for AH had higher overall survival compared to AC (94% vs 82%, p = 0.001) and NASH (94% vs 84%, p = 0.005).
Discussion: While disease recurrence after LT for NASH is higher than AC, but similar to AH, recipients of LT for AH had higher overall survival compared to recipients of LT for AC and NASH.

Figure: Figure 1. Primary Disease Relapse Rates After Liver Transplantation
Disclosures:
Smruti Rath indicated no relevant financial relationships.
Ishaan Dharia indicated no relevant financial relationships.
Gene Im indicated no relevant financial relationships.
Smruti Rath, MD1, Ishaan Dharia, MD2, Gene Im, MD3. P3853 - Disease Recurrence After Liver Transplantation for NASH Is Higher Than Alcohol-Associated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

