Tuesday Poster Session
Category: Biliary/Pancreas
P2853 - Prevalence of CFTR Pathogenic Variants in Pancreatitis: A Systematic Review and Meta-Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Joanna Jiang, MD
The Ohio State Wexner Medical Center
Columbus, OH
Presenting Author(s)
Joanna Jiang, MD1, Gavisha Waidyaratne, MD2, Shiab Mussad, MD1, Maegan E. Roberts, MS3, Yevgeniya Gokun, MS2, Spencer Harris, MS3, Peter P. Stanich, MD1, Phil Hart, MD4, Luis Lara, MD2, Somashekar Krishna, MD1, Peter Lee, MD1, Samuel Han, MD2, Georgios I. Papachristou, MD, PhD1, Mitchell Ramsey, MD1
1The Ohio State Wexner Medical Center, Columbus, OH; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3Ohio State University, Columbus, OH; 4The Ohio State University, Columbus, OH
Introduction: Pathogenic variants (PVs) in the cystic fibrosis transmembrane conductance regulator (CFTR) gene have been described as the most frequent genetic risk factor for pancreatitis. However, the prevalence of CFTR PVs across the spectrum of pancreatic disorders has not been fully characterized.
Methods: A systematic search was performed on 3/16/2022 in Pubmed and Embase, using synonyms for CFTR and pancreatitis. We included all manuscripts and abstracts published in English that reported the prevalence of CFTR PVs among human subjects with acute pancreatitis (AP), recurrent acute pancreatitis (RAP), chronic pancreatitis (CP), and pancreatitis not otherwise specified (NOS).
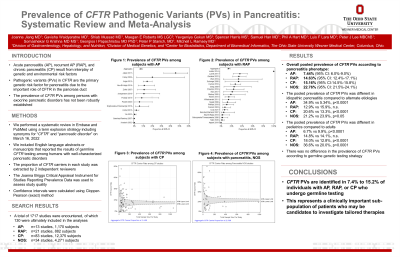
Results: The search strategy produced 1,281 studies published between 1998 and 2022. After excluding studies that did not meet inclusion criteria, 134 studies were ultimately included (Figure 1). The pooled prevalence of at least one CFTR PV is 87/1170 (7.4%) of AP, 132/882 (15.0%) of RAP, 1887/12472 (15.1%) of CP, and 978/4291 (22.8%) with pancreatitis NOS.
Subgroup analyses based on age category (pediatric vs adult) and etiology (idiopathic vs others) were performed. Among subjects with AP, there was no difference in the prevalence of CFTR PVs between pediatric and adult subjects, but subjects with idiopathic AP were more likely to have a CFTR PV than those with other etiologies (34.9% vs 5.34%, p< 0.001). Among subjects with RAP, there was no difference in the prevalence of CFTR PVs based on age category or etiology of pancreatitis. Among subjects with CP, the highest prevalence of CFTR PVs was seen in mixed age (18.3%) and pediatric studies (18.0%), followed by adult studies (12.8%) (p< 0.001). Idiopathic CP had nearly twice the prevalence of CFTR PVs compared to other etiologies (25.0% vs 13.2%, p< 0.001). Among subjects with pancreatitis NOS, the highest prevalence of CFTR PVs was seen in pediatric studies (36.6%), then adult (20.1%) and mixed age studies (17.9%) (p< 0.001). The prevalence of CFTR PVs was lower for idiopathic than other etiologies of pancreatitis NOS (20.6% vs 24.2%, p=0.004).
Discussion: The prevalence of CFTR PVs varies according to pancreatitis type, etiology, and subject age. Consideration to these demographic and clinical features can assist clinicians in whether to order genetic testing for CFTR, and generate estimates to guide pre-test decision making.

Disclosures:
Joanna Jiang, MD1, Gavisha Waidyaratne, MD2, Shiab Mussad, MD1, Maegan E. Roberts, MS3, Yevgeniya Gokun, MS2, Spencer Harris, MS3, Peter P. Stanich, MD1, Phil Hart, MD4, Luis Lara, MD2, Somashekar Krishna, MD1, Peter Lee, MD1, Samuel Han, MD2, Georgios I. Papachristou, MD, PhD1, Mitchell Ramsey, MD1. P2853 - Prevalence of CFTR Pathogenic Variants in Pancreatitis: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1The Ohio State Wexner Medical Center, Columbus, OH; 2The Ohio State University Wexner Medical Center, Columbus, OH; 3Ohio State University, Columbus, OH; 4The Ohio State University, Columbus, OH
Introduction: Pathogenic variants (PVs) in the cystic fibrosis transmembrane conductance regulator (CFTR) gene have been described as the most frequent genetic risk factor for pancreatitis. However, the prevalence of CFTR PVs across the spectrum of pancreatic disorders has not been fully characterized.
Methods: A systematic search was performed on 3/16/2022 in Pubmed and Embase, using synonyms for CFTR and pancreatitis. We included all manuscripts and abstracts published in English that reported the prevalence of CFTR PVs among human subjects with acute pancreatitis (AP), recurrent acute pancreatitis (RAP), chronic pancreatitis (CP), and pancreatitis not otherwise specified (NOS).
Results: The search strategy produced 1,281 studies published between 1998 and 2022. After excluding studies that did not meet inclusion criteria, 134 studies were ultimately included (Figure 1). The pooled prevalence of at least one CFTR PV is 87/1170 (7.4%) of AP, 132/882 (15.0%) of RAP, 1887/12472 (15.1%) of CP, and 978/4291 (22.8%) with pancreatitis NOS.
Subgroup analyses based on age category (pediatric vs adult) and etiology (idiopathic vs others) were performed. Among subjects with AP, there was no difference in the prevalence of CFTR PVs between pediatric and adult subjects, but subjects with idiopathic AP were more likely to have a CFTR PV than those with other etiologies (34.9% vs 5.34%, p< 0.001). Among subjects with RAP, there was no difference in the prevalence of CFTR PVs based on age category or etiology of pancreatitis. Among subjects with CP, the highest prevalence of CFTR PVs was seen in mixed age (18.3%) and pediatric studies (18.0%), followed by adult studies (12.8%) (p< 0.001). Idiopathic CP had nearly twice the prevalence of CFTR PVs compared to other etiologies (25.0% vs 13.2%, p< 0.001). Among subjects with pancreatitis NOS, the highest prevalence of CFTR PVs was seen in pediatric studies (36.6%), then adult (20.1%) and mixed age studies (17.9%) (p< 0.001). The prevalence of CFTR PVs was lower for idiopathic than other etiologies of pancreatitis NOS (20.6% vs 24.2%, p=0.004).
Discussion: The prevalence of CFTR PVs varies according to pancreatitis type, etiology, and subject age. Consideration to these demographic and clinical features can assist clinicians in whether to order genetic testing for CFTR, and generate estimates to guide pre-test decision making.

Figure: Figure 1: Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram
Disclosures:
Joanna Jiang indicated no relevant financial relationships.
Gavisha Waidyaratne indicated no relevant financial relationships.
Shiab Mussad indicated no relevant financial relationships.
Maegan Roberts: GeneDx (08/19/2013-04/01/2022) – Employee.
Yevgeniya Gokun indicated no relevant financial relationships.
Spencer Harris indicated no relevant financial relationships.
Peter Stanich: Freenome – Grant/Research Support. Guardant – Grant/Research Support. Janssen Pharma – Grant/Research Support. Pfizer Inc. – Grant/Research Support.
Phil Hart indicated no relevant financial relationships.
Luis Lara: AbbVie Inc. – Consultant, Speakers Bureau.
Somashekar Krishna: Mauna Kea Technologies – Grant/Research Support. Taewoong Medical USA – Grant/Research Support. US Biotest – Grant/Research Support.
Peter Lee indicated no relevant financial relationships.
Samuel Han indicated no relevant financial relationships.
Georgios Papachristou: AbbVie – Grant/Research Support. Nestlé – Speakers Bureau. Olympus – Consultant.
Mitchell Ramsey indicated no relevant financial relationships.
Joanna Jiang, MD1, Gavisha Waidyaratne, MD2, Shiab Mussad, MD1, Maegan E. Roberts, MS3, Yevgeniya Gokun, MS2, Spencer Harris, MS3, Peter P. Stanich, MD1, Phil Hart, MD4, Luis Lara, MD2, Somashekar Krishna, MD1, Peter Lee, MD1, Samuel Han, MD2, Georgios I. Papachristou, MD, PhD1, Mitchell Ramsey, MD1. P2853 - Prevalence of CFTR Pathogenic Variants in Pancreatitis: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

