Tuesday Poster Session
Category: Biliary/Pancreas
P2855 - Pancreatic Findings by Germline Mutation Status and Imaging Modality in Patients Undergoing Screening for Pancreatic Ductal Adenocarcinoma
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MS
Moniyka Sachar, MD
NYU Langone Health
New York, New York
Presenting Author(s)
Moniyka Sachar, MD1, Alexander Li, BA2, Alexander Prete, BA3, Eileen Janec, MD2, Gregory Haber, MD2, Lauren Khanna, MD3, Diane Simeone, MD2, Ahmad Al-Taee, MD2, Tamas Gonda, MD4
1NYU Langone Health, New York, NY; 2NYU, New York, NY; 3NYU Langone, New York, NY; 4NYU Grossman School of Medicine, New York, NY
Introduction: An estimated 10-15% of pancreatic ductal adenocarcinomas (PDAC) cases are attributable to genetic causes or are identified in patients with family history. Endoscopic Ultrasound (EUS) and Magnetic Resonance Imaging (MRI) are most sensitive modalities for screening in these high-risk individuals. Our goal was to identify the most common pancreatic EUS abnormalities in patients across genetic and familial risk factors and compare the prevalence of these findings in different mutation carriers at baseline and during surveillance.
Methods: We included participants undergoing index screening EUS between 2016 to 2021. Demographics, pathogenic germline mutation status (APC, BRCA1, BRCA2, PALB2, ATM, CHEK2, MLH1, MSH2, MSH6, STK11, CDKN2A, and PRSS1) and detailed pancreatic findings (cysts, masses, main pancreatic duct (MPD) dilation, and parenchymal changes) on initial and follow-up EUS and MRI were collected.
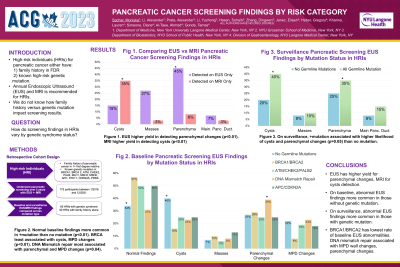
Results: Of 175 high-risk individuals (HRIs), 90 (51%) participants had family history alone (FHPC, control group) and 85 (49%) had a pathogenic germline mutation (GS). On baseline EUS and MRI screening, FHPC participants were more likely to have abnormal pancreatic findings (66% vs 50%; p = 0.03), including pancreatic cysts and MPD dilation than GS participants, with BRCA mutation associated with lowest risk of abnormalities at baseline (p< 0.01). 65 (37%) participants underwent surveillance EUS at > 2 years interval. On surveillance EUS screening, GS participants were more likely to have pancreatic abnormalities (44% vs 23%; p=0.05) than FHPC participants, with DNA mismatch repair mutations associated with the highest risk compared to other mutation statuses (p< 0.01). Parenchymal changes (45% vs 8%, p< 0.01) and MPD dilation (27% vs 3%; p< 0.01) were more frequently detected on EUS than MRI regardless of mutation status, whereas cysts < 10 mm were more frequently identified by MRI than EUS (35% vs 15%; p< 0.01).
Discussion: Our study is one of the largest to describe in detail pancreatic EUS and MRI findings by germline mutational status. Although parenchymal changes were less frequent in mutation carriers than in those without a known mutation, our results also show that certain germline mutation carriers develop parenchymal changes at a greater frequency.

Disclosures:
Moniyka Sachar, MD1, Alexander Li, BA2, Alexander Prete, BA3, Eileen Janec, MD2, Gregory Haber, MD2, Lauren Khanna, MD3, Diane Simeone, MD2, Ahmad Al-Taee, MD2, Tamas Gonda, MD4. P2855 - Pancreatic Findings by Germline Mutation Status and Imaging Modality in Patients Undergoing Screening for Pancreatic Ductal Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2NYU, New York, NY; 3NYU Langone, New York, NY; 4NYU Grossman School of Medicine, New York, NY
Introduction: An estimated 10-15% of pancreatic ductal adenocarcinomas (PDAC) cases are attributable to genetic causes or are identified in patients with family history. Endoscopic Ultrasound (EUS) and Magnetic Resonance Imaging (MRI) are most sensitive modalities for screening in these high-risk individuals. Our goal was to identify the most common pancreatic EUS abnormalities in patients across genetic and familial risk factors and compare the prevalence of these findings in different mutation carriers at baseline and during surveillance.
- Delete highlight and card
- Add a new card to this highlight
- Collect highlight and card
Methods: We included participants undergoing index screening EUS between 2016 to 2021. Demographics, pathogenic germline mutation status (APC, BRCA1, BRCA2, PALB2, ATM, CHEK2, MLH1, MSH2, MSH6, STK11, CDKN2A, and PRSS1) and detailed pancreatic findings (cysts, masses, main pancreatic duct (MPD) dilation, and parenchymal changes) on initial and follow-up EUS and MRI were collected.
- Delete highlight and card
- Add a new card to this highlight
- Collect highlight and card
Results: Of 175 high-risk individuals (HRIs), 90 (51%) participants had family history alone (FHPC, control group) and 85 (49%) had a pathogenic germline mutation (GS). On baseline EUS and MRI screening, FHPC participants were more likely to have abnormal pancreatic findings (66% vs 50%; p = 0.03), including pancreatic cysts and MPD dilation than GS participants, with BRCA mutation associated with lowest risk of abnormalities at baseline (p< 0.01). 65 (37%) participants underwent surveillance EUS at > 2 years interval. On surveillance EUS screening, GS participants were more likely to have pancreatic abnormalities (44% vs 23%; p=0.05) than FHPC participants, with DNA mismatch repair mutations associated with the highest risk compared to other mutation statuses (p< 0.01). Parenchymal changes (45% vs 8%, p< 0.01) and MPD dilation (27% vs 3%; p< 0.01) were more frequently detected on EUS than MRI regardless of mutation status, whereas cysts < 10 mm were more frequently identified by MRI than EUS (35% vs 15%; p< 0.01).
- Delete highlight and card
- Add a new card to this highlight
- Collect highlight and card
Discussion: Our study is one of the largest to describe in detail pancreatic EUS and MRI findings by germline mutational status. Although parenchymal changes were less frequent in mutation carriers than in those without a known mutation, our results also show that certain germline mutation carriers develop parenchymal changes at a greater frequency.
- Delete highlight and card
- Add a new card to this highlight
- Collect highlight and card

Figure: Title: Comparing Yield of Endoscopic Ultrasound (EUS) versus Magnetic Resonance Imaging (MRI) in Pancreatic Cancer Screening Across High-Risk Individuals (HRIs).
Caption: *P-values calculated via Chi-square Analysis.
Caption: *P-values calculated via Chi-square Analysis.
Disclosures:
Moniyka Sachar indicated no relevant financial relationships.
Alexander Li indicated no relevant financial relationships.
Alexander Prete indicated no relevant financial relationships.
Eileen Janec indicated no relevant financial relationships.
Gregory Haber: BSC – Consultant. Digma – Consultant. Erbe – Consultant. Medtronic – Consultant. Microtech – Consultant. Olympus – Consultant. Ovesco – Consultant.
Lauren Khanna indicated no relevant financial relationships.
Diane Simeone indicated no relevant financial relationships.
Ahmad Al-Taee indicated no relevant financial relationships.
Tamas Gonda indicated no relevant financial relationships.
Moniyka Sachar, MD1, Alexander Li, BA2, Alexander Prete, BA3, Eileen Janec, MD2, Gregory Haber, MD2, Lauren Khanna, MD3, Diane Simeone, MD2, Ahmad Al-Taee, MD2, Tamas Gonda, MD4. P2855 - Pancreatic Findings by Germline Mutation Status and Imaging Modality in Patients Undergoing Screening for Pancreatic Ductal Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
