Tuesday Poster Session
Category: Liver
P3855 - Disentangling Disparities in Hepatitis C - A Real-World Experience From Inside the Safety Net
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Landen Shane Burstiner, DO, MSc
University of Florida Health Jacksonville
Jacksonville, FL
Presenting Author(s)
Landen Shane Burstiner, DO, MSc1, Gregory Churchill, DO1, Avni Agrawal, DO1, Darby Oakes, MPH, DO2, Oshin Rai, DO1, Reshmi Mathew, DO1, Christopher Marsalisi, DO1, Abbey Johnston, PharmD1, Maged P. Ghali, MD3
1University of Florida Health Jacksonville, Jacksonville, FL; 2Broward Health Medical Center, Fort Lauderdale, FL; 3University of Florida, Jacksonville, FL
Introduction: Hepatitis C Virus is the most common bloodborne infection in the United States, with an estimated 2.7 million people infected. Highly efficacious oral medications often result in virologic cure in as little as 8-12 weeks, however, these medications are not easily accessible to all patients. From a public health perspective, it is of paramount importance to make treatment available to those most likely to transmit the virus; thus it behooves investigators to analyze and resolve any prohibitive obstacles to treatment.
Methods: In this retrospective study we exported information from electronic medical records of a tertiary care center in a medically underserved area on all patients that had a referral to an in-network hepatology clinic along with an international classification of disease code associated with HCV. Other patient details were exported and analyzed including sex, race, insurance, and completed hepatology clinic visits.
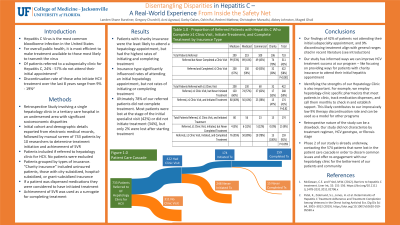
Results: From 2016 to 2023, 733 patients were referred to our hepatology clinics for HCV. Out of these, 422 (58%) were seen at least once in clinic, 174 (24%) started treatment, and 159 (22%) completed treatment. Insurance type had a statistically significant influence on the proportion of patients who attended at least one hepatology appointment (p < 0.001), but did not demonstrate a statistically significant influence on the proportion of patients who started (p = 0.82) nor completed treatment (p = 0.059). Race did significantly influence the appointment rate - the highest proportion of patients that completed at least one hepatology appointment were black (p < 0.001), but race did not impact the proportion starting or completing treatment. Sex did not significantly influence appointment rate, treatment initiation, or treatment completion.
Discussion: In a population with significant socioeconomic disparities, we can utilize these critical findings to initiate a targeted approach at improving access to HCV treatment. Charity patients have the lowest rate of completing a visit with a hepatologist, which represents an important obstacle to address. Of note, once a charity patient is seen, although not statistically significant, a higher proportion of them started and completed treatment than any other insurance class. Further studies aimed at exploring the source of referrals (for example, emergency room referrals vs referrals from a primary care provider) along with other demographic and social differences would be beneficial.
Disclosures:
Landen Shane Burstiner, DO, MSc1, Gregory Churchill, DO1, Avni Agrawal, DO1, Darby Oakes, MPH, DO2, Oshin Rai, DO1, Reshmi Mathew, DO1, Christopher Marsalisi, DO1, Abbey Johnston, PharmD1, Maged P. Ghali, MD3. P3855 - Disentangling Disparities in Hepatitis C - A Real-World Experience From Inside the Safety Net, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Florida Health Jacksonville, Jacksonville, FL; 2Broward Health Medical Center, Fort Lauderdale, FL; 3University of Florida, Jacksonville, FL
Introduction: Hepatitis C Virus is the most common bloodborne infection in the United States, with an estimated 2.7 million people infected. Highly efficacious oral medications often result in virologic cure in as little as 8-12 weeks, however, these medications are not easily accessible to all patients. From a public health perspective, it is of paramount importance to make treatment available to those most likely to transmit the virus; thus it behooves investigators to analyze and resolve any prohibitive obstacles to treatment.
Methods: In this retrospective study we exported information from electronic medical records of a tertiary care center in a medically underserved area on all patients that had a referral to an in-network hepatology clinic along with an international classification of disease code associated with HCV. Other patient details were exported and analyzed including sex, race, insurance, and completed hepatology clinic visits.
Results: From 2016 to 2023, 733 patients were referred to our hepatology clinics for HCV. Out of these, 422 (58%) were seen at least once in clinic, 174 (24%) started treatment, and 159 (22%) completed treatment. Insurance type had a statistically significant influence on the proportion of patients who attended at least one hepatology appointment (p < 0.001), but did not demonstrate a statistically significant influence on the proportion of patients who started (p = 0.82) nor completed treatment (p = 0.059). Race did significantly influence the appointment rate - the highest proportion of patients that completed at least one hepatology appointment were black (p < 0.001), but race did not impact the proportion starting or completing treatment. Sex did not significantly influence appointment rate, treatment initiation, or treatment completion.
Discussion: In a population with significant socioeconomic disparities, we can utilize these critical findings to initiate a targeted approach at improving access to HCV treatment. Charity patients have the lowest rate of completing a visit with a hepatologist, which represents an important obstacle to address. Of note, once a charity patient is seen, although not statistically significant, a higher proportion of them started and completed treatment than any other insurance class. Further studies aimed at exploring the source of referrals (for example, emergency room referrals vs referrals from a primary care provider) along with other demographic and social differences would be beneficial.
Disclosures:
Landen Shane Burstiner indicated no relevant financial relationships.
Gregory Churchill indicated no relevant financial relationships.
Avni Agrawal indicated no relevant financial relationships.
Darby Oakes indicated no relevant financial relationships.
Oshin Rai indicated no relevant financial relationships.
Reshmi Mathew indicated no relevant financial relationships.
Christopher Marsalisi indicated no relevant financial relationships.
Abbey Johnston indicated no relevant financial relationships.
Maged Ghali indicated no relevant financial relationships.
Landen Shane Burstiner, DO, MSc1, Gregory Churchill, DO1, Avni Agrawal, DO1, Darby Oakes, MPH, DO2, Oshin Rai, DO1, Reshmi Mathew, DO1, Christopher Marsalisi, DO1, Abbey Johnston, PharmD1, Maged P. Ghali, MD3. P3855 - Disentangling Disparities in Hepatitis C - A Real-World Experience From Inside the Safety Net, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
