Tuesday Poster Session
Category: Biliary/Pancreas
P2861 - The Effect of Pre-Diagnosis HbA1c and BMI on Pancreatic Cancer Staging at Diagnosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Sheena Bhushan, MD
Northeast Georgia Medical Center
Atlanta, GA
Presenting Author(s)
Sheena Bhushan, MD1, Tanya Aggarwal, MD2, Zainab Abbasi, MD2, Ange Ahoussougbemey, MD2, Shane Robinson, MS2, Riaz Mahmood, DO2
1Northeast Georgia Medical Center, Atlanta, GA; 2Northeast Georgia Medical Center, Gainesville, GA
Introduction: Introduction
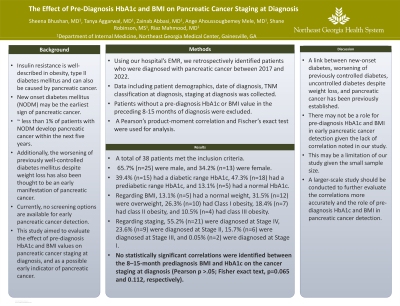
Insulin resistance is well-described in obesity, type II diabetes mellitus and can also be caused by pancreatic cancer. New onset diabetes mellitus (NODM) may be the earliest sign of pancreatic cancer, with less than 1% of patients developing pancreatic cancer within five years. Additionally, the worsening of previously well-controlled diabetes mellitus despite weight loss has also been thought to be an early manifestation of pancreatic cancer. Currently, no screening options are available for early pancreatic cancer detection. This study aimed to evaluate the effect of pre-diagnosis HbA1c and BMI values on pancreatic cancer staging at diagnosis.
Methods: Using our hospital cancer registry, we retrospectively identified patients who were diagnosed with pancreatic cancer between 2017 and 2022. Data including patient demographics, date of diagnosis, TNM classification at diagnosis, staging at diagnosis were collected. Patients without a pre-diagnosis HbA1c or BMI value in the preceding 8-15 months of diagnosis were excluded. A Pearson’s product-moment correlation and Fischer’s exact test were used for analysis.
Results: A total of 38 patients met the inclusion criteria. 65.7% (n=25) were male, and 36.8% (n=14) were female. 39.4% (n=15) had a diabetic range HbA1c, 47.3% (n=18) had a prediabetic range HbA1c, and 13.1% (n=5) had a normal HbA1c. Regarding BMI, 13.1% (n=5) had a normal weight, 31.5% (n=12) were overweight, 26.3% (n=10) had Class I obesity, 18.4% (n=7) had class II obesity, and 10.5% (n=4) had class III obesity. Regarding staging, 55.2% (n=21) were diagnosed at Stage IV, 23.6% (n=9) were diagnosed at Stage II, 15.7% (n=6) were diagnosed at Stage III, and 0.05% (n=2) were diagnosed at Stage 1. No statistically significant correlations were identified between the 8–15-month prediagnosis BMI and HbA1c on the cancer staging at diagnosis (Pearson p >.05; Fisher exact text, p=0.065 and 0.112, respectively).
Discussion: A link between new-onset diabetes, worsening of previously controlled diabetes, uncontrolled diabetes despite weight loss, and pancreatic cancer has been previously established. There may not be a role for pre-diagnosis HbA1c and BMI in early pancreatic cancer detection given the lack of correlation noted in our study. This may be a limitation of our study given the small sample size. A larger-scale study should be conducted to further evaluate the correlations more accurately and the role of pre- diagnosis HbA1c and BMI in pancreatic cancer detection.
Disclosures:
Sheena Bhushan, MD1, Tanya Aggarwal, MD2, Zainab Abbasi, MD2, Ange Ahoussougbemey, MD2, Shane Robinson, MS2, Riaz Mahmood, DO2. P2861 - The Effect of Pre-Diagnosis HbA1c and BMI on Pancreatic Cancer Staging at Diagnosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Northeast Georgia Medical Center, Atlanta, GA; 2Northeast Georgia Medical Center, Gainesville, GA
Introduction: Introduction
Insulin resistance is well-described in obesity, type II diabetes mellitus and can also be caused by pancreatic cancer. New onset diabetes mellitus (NODM) may be the earliest sign of pancreatic cancer, with less than 1% of patients developing pancreatic cancer within five years. Additionally, the worsening of previously well-controlled diabetes mellitus despite weight loss has also been thought to be an early manifestation of pancreatic cancer. Currently, no screening options are available for early pancreatic cancer detection. This study aimed to evaluate the effect of pre-diagnosis HbA1c and BMI values on pancreatic cancer staging at diagnosis.
Methods: Using our hospital cancer registry, we retrospectively identified patients who were diagnosed with pancreatic cancer between 2017 and 2022. Data including patient demographics, date of diagnosis, TNM classification at diagnosis, staging at diagnosis were collected. Patients without a pre-diagnosis HbA1c or BMI value in the preceding 8-15 months of diagnosis were excluded. A Pearson’s product-moment correlation and Fischer’s exact test were used for analysis.
Results: A total of 38 patients met the inclusion criteria. 65.7% (n=25) were male, and 36.8% (n=14) were female. 39.4% (n=15) had a diabetic range HbA1c, 47.3% (n=18) had a prediabetic range HbA1c, and 13.1% (n=5) had a normal HbA1c. Regarding BMI, 13.1% (n=5) had a normal weight, 31.5% (n=12) were overweight, 26.3% (n=10) had Class I obesity, 18.4% (n=7) had class II obesity, and 10.5% (n=4) had class III obesity. Regarding staging, 55.2% (n=21) were diagnosed at Stage IV, 23.6% (n=9) were diagnosed at Stage II, 15.7% (n=6) were diagnosed at Stage III, and 0.05% (n=2) were diagnosed at Stage 1. No statistically significant correlations were identified between the 8–15-month prediagnosis BMI and HbA1c on the cancer staging at diagnosis (Pearson p >.05; Fisher exact text, p=0.065 and 0.112, respectively).
Discussion: A link between new-onset diabetes, worsening of previously controlled diabetes, uncontrolled diabetes despite weight loss, and pancreatic cancer has been previously established. There may not be a role for pre-diagnosis HbA1c and BMI in early pancreatic cancer detection given the lack of correlation noted in our study. This may be a limitation of our study given the small sample size. A larger-scale study should be conducted to further evaluate the correlations more accurately and the role of pre- diagnosis HbA1c and BMI in pancreatic cancer detection.
Disclosures:
Sheena Bhushan indicated no relevant financial relationships.
Tanya Aggarwal indicated no relevant financial relationships.
Zainab Abbasi indicated no relevant financial relationships.
Ange Ahoussougbemey indicated no relevant financial relationships.
Shane Robinson indicated no relevant financial relationships.
Riaz Mahmood indicated no relevant financial relationships.
Sheena Bhushan, MD1, Tanya Aggarwal, MD2, Zainab Abbasi, MD2, Ange Ahoussougbemey, MD2, Shane Robinson, MS2, Riaz Mahmood, DO2. P2861 - The Effect of Pre-Diagnosis HbA1c and BMI on Pancreatic Cancer Staging at Diagnosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
