Tuesday Poster Session
Category: Biliary/Pancreas
P2869 - Trends and Impact of EUS Utilization for Pancreatic Cysts Over Time
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- LW
Lillian Wang, MD
Mayo Clinic
Rochester, Minnesota
Presenting Author(s)
Lillian Wang, MD1, Priyanka Vatsavayi, MBBS1, Ferga Gleeson, MBBCh1, Shounak Majumder, MD1, Shifa Umar, MD2, Saran Velaga, MBBS1, Elizabeth Rajan, MD1, Barham Abu Dayyeh, MD, MPH1, Andrew Storm, MD1, Santhi Vege, MD1, Vinay Chandrasekhara, MD1
1Mayo Clinic, Rochester, MN; 2University of Chicago, Chicago, IL
Introduction: Multiple guidelines have been published to improve risk stratification and resource utilization for the management of neoplastic pancreatic cysts (PC). This study aims to evaluate trends in endoscopic ultrasound (EUS) utilization and assess agreement between pre-EUS cross-sectional imaging and EUS for specific PC features.
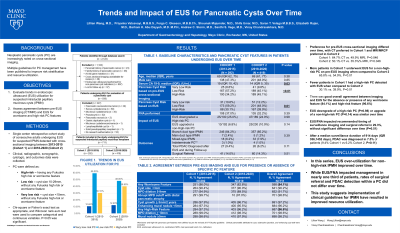
Methods: This single-center retrospective cohort study included consecutive adults undergoing EUS for suspected intraductal papillary mucinous neoplasms seen on cross-sectional imaging (CT/MR) between 2013-2015 (Cohort 1) and 2018-2020 (Cohort 2). Patients without CT/MR and those undergoing EUS for non-PC indications were excluded. Clinical, imaging, cytologic and outcomes data were collected. PC were defined as high-risk (having any Fukuoka high risk (HR) or worrisome feature (WF)), low risk (cyst size 10-29mm, without any HR or WF), and very low risk (cyst size < 10mm, without any HR or WF). Chi-square or Fisher’s exact test and Wilcoxon rank-sum test were used to compare categorical and continuous variables. P< 0.05 was significant.
Results: Of 711 included patients, 292 (41.1%) were in Cohort 1. Pre-EUS cross-sectional imaging differed over time, with CT preferred in Cohort 1 (64.7% vs 49.9%, P=0.046) and MRCP/MRI in Cohort 2 (50.1% vs 35.3%, P=0.046). More patients in Cohort 1 underwent EUS for non-high-risk PC on pre-EUS imaging (65.8% vs 54.9%, P< 0.01). Fewer patients in Cohort 1 had a high-risk PC detected with EUS compared to Cohort 2 (30.1% vs 39.9%, P=0.01). Median baseline CA 19-9 was significantly higher in Cohort 1 (P=0.03). Other baseline characteristics were similar (Table 1). Fine needle aspiration (FNA) was performed in 34.2% and did not change over time. Overall, there was good agreement between CT/MR and EUS for the absence or presence of any WF (84.1%) and HR features (96.6%). EUS downgraded a high-risk PC in 24.9% and upgraded a non-high-risk PC in 9.0% and remained stable over time. EUS/FNA impacted recommended timing of index surveillance imaging and surgical referral in 29.3% patients, without significant difference over time. Median surveillance duration was 914 days (IQR 356, 1452 days), during which pancreatic ductal adenocarcinoma (PDAC) diagnosed in 7.5% of patients (9.4% Cohort 1 vs 6.2% Cohort 2, P=0.11).
Discussion: In this series, EUS over-utilization for low-risk PC improved over time. EUS changed management in 29.3% of patients, without change over time or impacting rate of PDAC diagnosis.

Disclosures:
Lillian Wang, MD1, Priyanka Vatsavayi, MBBS1, Ferga Gleeson, MBBCh1, Shounak Majumder, MD1, Shifa Umar, MD2, Saran Velaga, MBBS1, Elizabeth Rajan, MD1, Barham Abu Dayyeh, MD, MPH1, Andrew Storm, MD1, Santhi Vege, MD1, Vinay Chandrasekhara, MD1. P2869 - Trends and Impact of EUS Utilization for Pancreatic Cysts Over Time, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2University of Chicago, Chicago, IL
Introduction: Multiple guidelines have been published to improve risk stratification and resource utilization for the management of neoplastic pancreatic cysts (PC). This study aims to evaluate trends in endoscopic ultrasound (EUS) utilization and assess agreement between pre-EUS cross-sectional imaging and EUS for specific PC features.
Methods: This single-center retrospective cohort study included consecutive adults undergoing EUS for suspected intraductal papillary mucinous neoplasms seen on cross-sectional imaging (CT/MR) between 2013-2015 (Cohort 1) and 2018-2020 (Cohort 2). Patients without CT/MR and those undergoing EUS for non-PC indications were excluded. Clinical, imaging, cytologic and outcomes data were collected. PC were defined as high-risk (having any Fukuoka high risk (HR) or worrisome feature (WF)), low risk (cyst size 10-29mm, without any HR or WF), and very low risk (cyst size < 10mm, without any HR or WF). Chi-square or Fisher’s exact test and Wilcoxon rank-sum test were used to compare categorical and continuous variables. P< 0.05 was significant.
Results: Of 711 included patients, 292 (41.1%) were in Cohort 1. Pre-EUS cross-sectional imaging differed over time, with CT preferred in Cohort 1 (64.7% vs 49.9%, P=0.046) and MRCP/MRI in Cohort 2 (50.1% vs 35.3%, P=0.046). More patients in Cohort 1 underwent EUS for non-high-risk PC on pre-EUS imaging (65.8% vs 54.9%, P< 0.01). Fewer patients in Cohort 1 had a high-risk PC detected with EUS compared to Cohort 2 (30.1% vs 39.9%, P=0.01). Median baseline CA 19-9 was significantly higher in Cohort 1 (P=0.03). Other baseline characteristics were similar (Table 1). Fine needle aspiration (FNA) was performed in 34.2% and did not change over time. Overall, there was good agreement between CT/MR and EUS for the absence or presence of any WF (84.1%) and HR features (96.6%). EUS downgraded a high-risk PC in 24.9% and upgraded a non-high-risk PC in 9.0% and remained stable over time. EUS/FNA impacted recommended timing of index surveillance imaging and surgical referral in 29.3% patients, without significant difference over time. Median surveillance duration was 914 days (IQR 356, 1452 days), during which pancreatic ductal adenocarcinoma (PDAC) diagnosed in 7.5% of patients (9.4% Cohort 1 vs 6.2% Cohort 2, P=0.11).
Discussion: In this series, EUS over-utilization for low-risk PC improved over time. EUS changed management in 29.3% of patients, without change over time or impacting rate of PDAC diagnosis.

Figure: Figure 1. Flow Diagram of Cohort Creation.
Legend: EUS, endoscopic ultrasound
Legend: EUS, endoscopic ultrasound
Disclosures:
Lillian Wang indicated no relevant financial relationships.
Priyanka Vatsavayi indicated no relevant financial relationships.
Ferga Gleeson indicated no relevant financial relationships.
Shounak Majumder: Exact Sciences – Grant/Research Support, Intellectual Property/Patents.
Shifa Umar indicated no relevant financial relationships.
Saran Velaga indicated no relevant financial relationships.
Elizabeth Rajan: Medtronic – Intellectual Property/Patents, Royalties. Olympus – Consultant. Ruhoff – Intellectual Property/Patents, Royalties.
Barham Abu Dayyeh: Apollo Endosurgery – Consultant, Grant/Research Support. Aspire Bariatrics – Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cairn Diagnostics – Grant/Research Support. DyaMx – Consultant. Endogastric Solutions – Speakers Bureau. Endo-TAGSS – Consultant. GI Dynamics – Grant/Research Support. Johnson and Johnson – Speakers Bureau. Medtronic – Grant/Research Support. Olympus – Speakers Bureau. Spatz Medical – Grant/Research Support. USGI Medical – Consultant, Grant/Research Support.
Andrew Storm: Apollo – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Endogenex – Consultant, Grant/Research Support. Endo-TAGSS – Consultant. Enterasense – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant, Grant/Research Support. MGI Medical – Consultant. Microtech – Consultant. Olypmus – Consultant. OnePass – Grant/Research Support. Pillsense – Consultant, Grant/Research Support.
Santhi Vege: UpToDate – Royalties.
Vinay Chandrasekhara: Boston Scientific – Consultant. Covidien LP – Consultant. Micro-Tech Endoscopy – Grant/Research Support. Nevakar Corp – Stock Options.
Lillian Wang, MD1, Priyanka Vatsavayi, MBBS1, Ferga Gleeson, MBBCh1, Shounak Majumder, MD1, Shifa Umar, MD2, Saran Velaga, MBBS1, Elizabeth Rajan, MD1, Barham Abu Dayyeh, MD, MPH1, Andrew Storm, MD1, Santhi Vege, MD1, Vinay Chandrasekhara, MD1. P2869 - Trends and Impact of EUS Utilization for Pancreatic Cysts Over Time, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

