Tuesday Poster Session
Category: Liver
P3874 - Non-Hepatic Hyperammonemic Encephalopathy: An Unmasked Urea Cycle Disorder in the Setting of Late Gastric Bypass Complication
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- RZ
Rached Zeghlache, BSc, MD
Waterbury Hospital
Waterbury, CT
Presenting Author(s)
Rached Zeghlache, BSc, MD, Tijana Samardzic, MD, Katelyn Norman, MD
Waterbury Hospital, Waterbury, CT
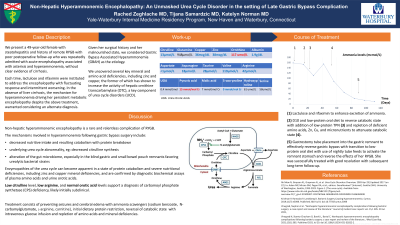
Introduction: Non-hepatic hyperammonemic encephalopathy is a rare complication of Roux-en-Y gastric bypass (RYGB) surgery. The pathogenesis is seemingly multifactorial, related to previously subclinical urea cycle disorders. It has a high morbidity and takes significant metabolic control to prevent recurrent encephalopathy.
Case Description/Methods: We present a 49-year-old female with steatohepatitis and history of remote RYGB with poor postoperative follow-up and malnutrition. She was repeatedly admitted with acute encephalopathy associated with asterixis and hyperammonemia, without clear evidence of cirrhosis. Each time, lactulose and rifaximin were instituted with limited response. The Persistence of her encephalopathy despite usual treatment warranted consideration for an alternate diagnosis, specifically Gastric Bypass Associated Hyperammonemia (GBAH). We uncovered several key mineral and amino acid deficiencies, including zinc which has been shown to increase the activity of hepatic ornithine transcarbamylase (OTC), a critical actor in urea cycle disorders (UCD).
Acutely, she was treated with IV dextrose to reverse the catabolic state of her acute illness, minimizing ammonia production. She was given lactulose to increase ammonia clearance, and rifaximin to reduce intestinal burden of ammonia producing bacteria. Once ammonia levels stabilized, low-protein TPN with trace elements, was initiated.
Surgical reversal of the RYGB was considered but abandoned in favor of gastrostomy tube to the remnant stomach, effectively reversing the previous bypass. TPN was discontinued with transition to a low-protein oral diet with nightly tube feeds to recruit the remnant stomach. Laboratory evidence of malnutrition improved, and the encephalopathy resolved.
Discussion: Accumulation of ammonia may occur due to excessive catabolic protein degradation, liver dysfunction, enzymatic UCD, and ammonia-producing bacterial overgrowth. In the case of GBAH, previously subclinical UCDs may be unmasked by amino acid and mineral deficiencies as well as significant muscle wasting, and bacterial overgrowth within the bypass remnant. Our patient fits this clinical syndrome and the existence of a UCD was supported by a low citrulline and elevated glutamine which are seen late-onset OTC deficiencies.
While urea cycle enzymopathies are more common in the pediatric population, underlying functional deficiencies may become apparent in this setting and should therefore be considered as a cause for acute hyperammonemic encephalopathy.
Disclosures:
Rached Zeghlache, BSc, MD, Tijana Samardzic, MD, Katelyn Norman, MD. P3874 - Non-Hepatic Hyperammonemic Encephalopathy: An Unmasked Urea Cycle Disorder in the Setting of Late Gastric Bypass Complication, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Waterbury Hospital, Waterbury, CT
Introduction: Non-hepatic hyperammonemic encephalopathy is a rare complication of Roux-en-Y gastric bypass (RYGB) surgery. The pathogenesis is seemingly multifactorial, related to previously subclinical urea cycle disorders. It has a high morbidity and takes significant metabolic control to prevent recurrent encephalopathy.
Case Description/Methods: We present a 49-year-old female with steatohepatitis and history of remote RYGB with poor postoperative follow-up and malnutrition. She was repeatedly admitted with acute encephalopathy associated with asterixis and hyperammonemia, without clear evidence of cirrhosis. Each time, lactulose and rifaximin were instituted with limited response. The Persistence of her encephalopathy despite usual treatment warranted consideration for an alternate diagnosis, specifically Gastric Bypass Associated Hyperammonemia (GBAH). We uncovered several key mineral and amino acid deficiencies, including zinc which has been shown to increase the activity of hepatic ornithine transcarbamylase (OTC), a critical actor in urea cycle disorders (UCD).
Acutely, she was treated with IV dextrose to reverse the catabolic state of her acute illness, minimizing ammonia production. She was given lactulose to increase ammonia clearance, and rifaximin to reduce intestinal burden of ammonia producing bacteria. Once ammonia levels stabilized, low-protein TPN with trace elements, was initiated.
Surgical reversal of the RYGB was considered but abandoned in favor of gastrostomy tube to the remnant stomach, effectively reversing the previous bypass. TPN was discontinued with transition to a low-protein oral diet with nightly tube feeds to recruit the remnant stomach. Laboratory evidence of malnutrition improved, and the encephalopathy resolved.
Discussion: Accumulation of ammonia may occur due to excessive catabolic protein degradation, liver dysfunction, enzymatic UCD, and ammonia-producing bacterial overgrowth. In the case of GBAH, previously subclinical UCDs may be unmasked by amino acid and mineral deficiencies as well as significant muscle wasting, and bacterial overgrowth within the bypass remnant. Our patient fits this clinical syndrome and the existence of a UCD was supported by a low citrulline and elevated glutamine which are seen late-onset OTC deficiencies.
While urea cycle enzymopathies are more common in the pediatric population, underlying functional deficiencies may become apparent in this setting and should therefore be considered as a cause for acute hyperammonemic encephalopathy.
Disclosures:
Rached Zeghlache indicated no relevant financial relationships.
Tijana Samardzic indicated no relevant financial relationships.
Katelyn Norman indicated no relevant financial relationships.
Rached Zeghlache, BSc, MD, Tijana Samardzic, MD, Katelyn Norman, MD. P3874 - Non-Hepatic Hyperammonemic Encephalopathy: An Unmasked Urea Cycle Disorder in the Setting of Late Gastric Bypass Complication, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
