Tuesday Poster Session
Category: Biliary/Pancreas
P2875 - Can Pancreatic Cyst Detection Ratio Function as a Quality Indicator for EUS-Based Pancreatic Cancer Screening? A Systematic Review and Meta-Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- AC
Ankit Chhoda, MD
Beth Israel Deaconess Medical Center
Boston, MA
Presenting Author(s)
Ankit Chhoda, MD1, Maria Hernandez Woodbine, MD1, Andy Silva-Santisteban, MD2, Alyssa Grimshaw, MBA3, Craig Gunderson, MD4, James J. Farrell, MD5, Mandeep Sawhney, MD, MS1
1Beth Israel Deaconess Medical Center, Boston, MA; 2Beth Israel Deaconess Medical Center, Brighton, MA; 3Yale University Libraries, West Haven, CT; 4Yale School of Medicine, West Haven, CT; 5Yale School of Medicine, New Haven, CT
Introduction: Endoscopic ultrasound (EUS) is highly operator dependent, and almost all pancreatic cancer studies thus far have been performed at tertiary care centers with large variations in outcomes. Quality indicators (QI) can drive quality improvement in healthcare services. We sought to determine the prevalence and characteristics of pancreatic cysts and the proportion of pancreatic cancers found during the screening that originated from pancreatic cysts.
Methods: We identified and assessed pancreatic cystic lesions (PCLs) routinely noted on pancreatic cancer screening EUS for their suitability to serve as intermediate-outcome QIs. Using an iterative process, we determined that a pancreatic cyst-based QI would be optimal. We then conducted a systematic search (CRD42018117189) of Cochrane Library, Embase, Google Scholar, Medline, PubMed, Scopus, and Web of Science of pancreatic cancer screening studies to determine prevalence, characteristics, and malignant potential of PCLs in high-risk individuals (HRI). Cumulative effect sizes were calculated through meta-analysis of proportions using a random-effects model.
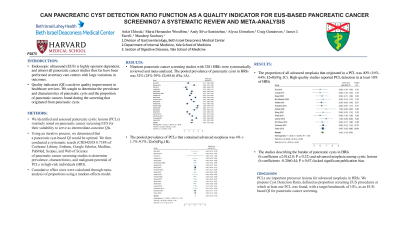
Results: Nineteen pancreatic cancer screening studies with 3281 HRIs were systematically reviewed and meta-analyzed. The pooled prevalence of pancreatic cysts in HRIs was 32% (25%-39%; I2=95.6) (Fig.1A). The pooled prevalence of PCLs that contained advanced neoplasia was 4% (-1.7%-9.7%; I2=0)(Fig.1B). The proportion of all advanced neoplasia that originated in a PCL was 40% (16%-64%; I2=0)(Fig.1C). High-quality studies reported PCL detection in at least 10% of HRIs. The studies describing the burden of pancreatic cysts in HRIs (b coefficient =2.01±2.0; P = 0.32) and advanced neoplasia among cystic lesions (b coefficient= -0.20±0.44; P = 0.67) lacked significant publication bias.
Discussion: PCLs are important precursor lesions for advanced neoplasia in HRIs. We propose Cyst Detection Ratio, defined as proportion screening EUS procedures at which at least one PCL was found, with a target benchmark of 10%, as an EUS-based QI for pancreatic cancer screening.

Disclosures:
Ankit Chhoda, MD1, Maria Hernandez Woodbine, MD1, Andy Silva-Santisteban, MD2, Alyssa Grimshaw, MBA3, Craig Gunderson, MD4, James J. Farrell, MD5, Mandeep Sawhney, MD, MS1. P2875 - Can Pancreatic Cyst Detection Ratio Function as a Quality Indicator for EUS-Based Pancreatic Cancer Screening? A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Boston, MA; 2Beth Israel Deaconess Medical Center, Brighton, MA; 3Yale University Libraries, West Haven, CT; 4Yale School of Medicine, West Haven, CT; 5Yale School of Medicine, New Haven, CT
Introduction: Endoscopic ultrasound (EUS) is highly operator dependent, and almost all pancreatic cancer studies thus far have been performed at tertiary care centers with large variations in outcomes. Quality indicators (QI) can drive quality improvement in healthcare services. We sought to determine the prevalence and characteristics of pancreatic cysts and the proportion of pancreatic cancers found during the screening that originated from pancreatic cysts.
Methods: We identified and assessed pancreatic cystic lesions (PCLs) routinely noted on pancreatic cancer screening EUS for their suitability to serve as intermediate-outcome QIs. Using an iterative process, we determined that a pancreatic cyst-based QI would be optimal. We then conducted a systematic search (CRD42018117189) of Cochrane Library, Embase, Google Scholar, Medline, PubMed, Scopus, and Web of Science of pancreatic cancer screening studies to determine prevalence, characteristics, and malignant potential of PCLs in high-risk individuals (HRI). Cumulative effect sizes were calculated through meta-analysis of proportions using a random-effects model.
Results: Nineteen pancreatic cancer screening studies with 3281 HRIs were systematically reviewed and meta-analyzed. The pooled prevalence of pancreatic cysts in HRIs was 32% (25%-39%; I2=95.6) (Fig.1A). The pooled prevalence of PCLs that contained advanced neoplasia was 4% (-1.7%-9.7%; I2=0)(Fig.1B). The proportion of all advanced neoplasia that originated in a PCL was 40% (16%-64%; I2=0)(Fig.1C). High-quality studies reported PCL detection in at least 10% of HRIs. The studies describing the burden of pancreatic cysts in HRIs (b coefficient =2.01±2.0; P = 0.32) and advanced neoplasia among cystic lesions (b coefficient= -0.20±0.44; P = 0.67) lacked significant publication bias.
Discussion: PCLs are important precursor lesions for advanced neoplasia in HRIs. We propose Cyst Detection Ratio, defined as proportion screening EUS procedures at which at least one PCL was found, with a target benchmark of 10%, as an EUS-based QI for pancreatic cancer screening.

Figure: Figure 1: (A)Forest Plot depicting cyst detection rate among all pancreatic cancer surveillance studies; (B) Incident advanced neoplasia among cystic lesions (C) Cyst-related advanced neoplasia of all advanced neoplasia.
Disclosures:
Ankit Chhoda indicated no relevant financial relationships.
Maria Hernandez Woodbine indicated no relevant financial relationships.
Andy Silva-Santisteban indicated no relevant financial relationships.
Alyssa Grimshaw indicated no relevant financial relationships.
Craig Gunderson indicated no relevant financial relationships.
James J. Farrell indicated no relevant financial relationships.
Mandeep Sawhney: Allurion – Stock Options. Immunovia Inc. – Consultant. Marlborough, MA – Consultant.
Ankit Chhoda, MD1, Maria Hernandez Woodbine, MD1, Andy Silva-Santisteban, MD2, Alyssa Grimshaw, MBA3, Craig Gunderson, MD4, James J. Farrell, MD5, Mandeep Sawhney, MD, MS1. P2875 - Can Pancreatic Cyst Detection Ratio Function as a Quality Indicator for EUS-Based Pancreatic Cancer Screening? A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
