Tuesday Poster Session
Category: Biliary/Pancreas
P2878 - Health Insurance Prevalence & Acute Pancreatitis Mortality: A Cross-Sectional Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Macklin Loveland, MD
University of Arizona College of Medicine
Tucson, AZ
Presenting Author(s)
Macklin Loveland, MD1, Elise Le Cam, MD2, Richard Trieu, MD1, Ala Kasrawi, MD3, Ramzi Ibrahim, MD4, Joao Paulo Albuquerque Ferreira, MD4
1University of Arizona College of Medicine, Tucson, AZ; 2University of Arizona–Banner University Medical Center, Tucson, AZ; 3Jordanian Royal Medical Services, Amman, 'Amman, Jordan; 4University of Arizona, Tucson, AZ
Introduction: Many people in the United States (US) lack healthcare coverage, which affects the prevention and management of many conditions. Healthcare spending for acute pancreatitis has significantly increased over the years. Considering the substantial morbidity and mortality associated with acute pancreatitis, we investigated the association between US county-level healthcare coverage prevalence and acute pancreatitis mortality rates.
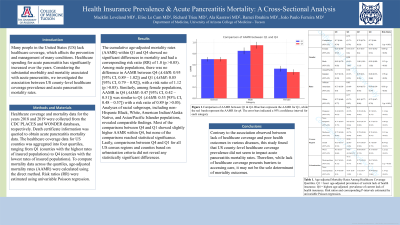
Methods: Healthcare coverage and mortality data for the years 2018 and 2019 were collected from the CDC PLACES and WONDER databases, respectively. Death certificate information was queried to obtain acute pancreatitis mortality data. The healthcare coverage data for US counties was aggregated into four quartiles, ranging from Q1 (counties with the highest rates of insured populations) to Q4 (counties with the lowest rates of insured populations). To compare mortality data across the quartiles, age-adjusted mortality rates (AAMR) were calculated using the direct method. Risk ratios (RR) were estimated using uni-variable Poisson regression.
Results: The cumulative age-adjusted mortality rates (AAMR) within Q1 and Q4 showed no significant differences in mortality and had a corresponding risk ratio (RR) of 1.0 (p >0.05). Among male populations, there was no difference in AAMR between Q4 (AAMR: 0.95 [95% CI, 0.89 – 1.02]) and Q1 (AAMR: 0.85 [95% CI, 0.79 – 0.92]), with a risk ratio of 1.12 (p >0.05). Similarly, among female populations, AAMR in Q4 (AAMR: 0.47 [95% CI, 0.42 – 0.51]) was similar to Q1 (AAMR: 0.53 [95% CI, 0.48 – 0.57]) with a risk ratio of 0.89 (p >0.05). Analyses of racial subgroups, including non-Hispanic Black, White, American Indian/Alaska Native, and Asian/Pacific Islander populations, revealed comparable findings. Most of the comparisons between Q4 and Q1 showed slightly higher AAMR within Q4, but none of the comparisons reached statistical significance. Lastly, comparisons between Q4 and Q1 for all US census regions and counties based on urbanization criteria did not reveal any statistically significant differences.
Discussion: Contrary to the association observed between lack of healthcare coverage and poor health outcomes in various diseases, this study found that US county-level healthcare coverage prevalence did not seem to impact acute pancreatitis mortality rates. Therefore, while lack of healthcare coverage presents barriers to accessing care, it may not be the sole determinant of mortality outcomes.
Disclosures:
Macklin Loveland, MD1, Elise Le Cam, MD2, Richard Trieu, MD1, Ala Kasrawi, MD3, Ramzi Ibrahim, MD4, Joao Paulo Albuquerque Ferreira, MD4. P2878 - Health Insurance Prevalence & Acute Pancreatitis Mortality: A Cross-Sectional Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Arizona College of Medicine, Tucson, AZ; 2University of Arizona–Banner University Medical Center, Tucson, AZ; 3Jordanian Royal Medical Services, Amman, 'Amman, Jordan; 4University of Arizona, Tucson, AZ
Introduction: Many people in the United States (US) lack healthcare coverage, which affects the prevention and management of many conditions. Healthcare spending for acute pancreatitis has significantly increased over the years. Considering the substantial morbidity and mortality associated with acute pancreatitis, we investigated the association between US county-level healthcare coverage prevalence and acute pancreatitis mortality rates.
Methods: Healthcare coverage and mortality data for the years 2018 and 2019 were collected from the CDC PLACES and WONDER databases, respectively. Death certificate information was queried to obtain acute pancreatitis mortality data. The healthcare coverage data for US counties was aggregated into four quartiles, ranging from Q1 (counties with the highest rates of insured populations) to Q4 (counties with the lowest rates of insured populations). To compare mortality data across the quartiles, age-adjusted mortality rates (AAMR) were calculated using the direct method. Risk ratios (RR) were estimated using uni-variable Poisson regression.
Results: The cumulative age-adjusted mortality rates (AAMR) within Q1 and Q4 showed no significant differences in mortality and had a corresponding risk ratio (RR) of 1.0 (p >0.05). Among male populations, there was no difference in AAMR between Q4 (AAMR: 0.95 [95% CI, 0.89 – 1.02]) and Q1 (AAMR: 0.85 [95% CI, 0.79 – 0.92]), with a risk ratio of 1.12 (p >0.05). Similarly, among female populations, AAMR in Q4 (AAMR: 0.47 [95% CI, 0.42 – 0.51]) was similar to Q1 (AAMR: 0.53 [95% CI, 0.48 – 0.57]) with a risk ratio of 0.89 (p >0.05). Analyses of racial subgroups, including non-Hispanic Black, White, American Indian/Alaska Native, and Asian/Pacific Islander populations, revealed comparable findings. Most of the comparisons between Q4 and Q1 showed slightly higher AAMR within Q4, but none of the comparisons reached statistical significance. Lastly, comparisons between Q4 and Q1 for all US census regions and counties based on urbanization criteria did not reveal any statistically significant differences.
Discussion: Contrary to the association observed between lack of healthcare coverage and poor health outcomes in various diseases, this study found that US county-level healthcare coverage prevalence did not seem to impact acute pancreatitis mortality rates. Therefore, while lack of healthcare coverage presents barriers to accessing care, it may not be the sole determinant of mortality outcomes.
Disclosures:
Macklin Loveland indicated no relevant financial relationships.
Elise Le Cam indicated no relevant financial relationships.
Richard Trieu indicated no relevant financial relationships.
Ala Kasrawi indicated no relevant financial relationships.
Ramzi Ibrahim indicated no relevant financial relationships.
Joao Paulo Albuquerque Ferreira indicated no relevant financial relationships.
Macklin Loveland, MD1, Elise Le Cam, MD2, Richard Trieu, MD1, Ala Kasrawi, MD3, Ramzi Ibrahim, MD4, Joao Paulo Albuquerque Ferreira, MD4. P2878 - Health Insurance Prevalence & Acute Pancreatitis Mortality: A Cross-Sectional Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
