Tuesday Poster Session
Category: Biliary/Pancreas
P2879 - Predictors of Idiopathic Common Bile Duct Dilatation: A Case-Control Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Iyiad Alabdul Razzak, MD
St. Elizabeth's Medical Center
Brighton, MA
Presenting Author(s)
Butros Fakhoury, MD1, Marcel Robles, MD2, Iyiad Alabdul Razzak, MD3, Tiago Barroso Vieira Costa, MD4, Syed K. Mahmood, MD, MPH3, Sandeep Krishnan, MD, PhD3
1St. Elizabeth's Medical Center, Birghton, ME; 2St. Elizabeth Medical Center, Brighton, MA; 3St. Elizabeth's Medical Center, Brighton, MA; 4St. Elizabeth's Medical Center, Boston, MA
Introduction: Common bile duct (CBD) dilation is occasionally encountered during workup for abdominal pain or identified incidentally on imaging studies. Endoscopic ultrasound (EUS) and Endoscopic retrograde cholangiopancreatography (ERCP) are often obtained to establish a diagnosis in these scenarios. However, a significant number of patients still do not have a known underlying cause for CBD dilation. This research aims to uncover the risk factors linked to idiopathic CBD dilation.
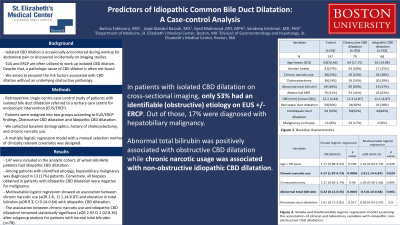
Methods: This is a retrospective case-control study of patients with isolated bile duct dilatation who were referred to a tertiary care center for EUS/ERCP. Patients were assigned into two groups according to EUS/ERCP findings, idiopathic CBD dilatation and CBD dilatation with identified etiology. Demographics including age and sex were obtained for each patient. History of cholecystectomy was obtained by reviewing the Imaging study at the time of diagnosis. Patients with chronic narcotic use were identified by the following methods: (1) Prescription for methadone or suboxone (2) Opiate prescription for at least 3 months during the year prior to the ERCP/EUS study. A multiple logistic regression model with a manual selection method of clinically relevant covariates including age > 60, history of cholecystectomy, abnormal total bilirubin, and pancreatic duct dilatation was designed. Sub-group analysis for patients with normal total bilirubin to adjust for confounders.
Results: After the application of selection criteria, 147 were included in the analytic cohort, of whom 68 (46%) patients had idiopathic CBD dilatation. Among patients with identified etiology, hepatobiliary malignancy was diagnosed in 13 (17%) patients and manifested as a suspicious stricture, ampullary or pancreatic lesion. On the other hand, all biopsies obtained in patients with idiopathic CBD dilatation were negative for malignancy. Multivariable logistic regression showed an association between chronic narcotic use aOR 2.8 CI 1.14-6.87 and elevation in total bilirubin aOR 0.3 CI 0.14-0.64 with idiopathic CBD dilatation. The association between Chronic narcotic usage and idiopathic CBD dilatation remained statistically significant aOR 2.92 CI 1.02-8.36 after subgroup analysis for patients with normal total bilirubin (N=78).
Discussion: Abnormal total bilirubin is inversely associated with idiopathic CBD dilatation and Chronic narcotic use is positively associated with idiopathic CBD dilatation even in patients with normal total bilirubin.
Disclosures:
Butros Fakhoury, MD1, Marcel Robles, MD2, Iyiad Alabdul Razzak, MD3, Tiago Barroso Vieira Costa, MD4, Syed K. Mahmood, MD, MPH3, Sandeep Krishnan, MD, PhD3. P2879 - Predictors of Idiopathic Common Bile Duct Dilatation: A Case-Control Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. Elizabeth's Medical Center, Birghton, ME; 2St. Elizabeth Medical Center, Brighton, MA; 3St. Elizabeth's Medical Center, Brighton, MA; 4St. Elizabeth's Medical Center, Boston, MA
Introduction: Common bile duct (CBD) dilation is occasionally encountered during workup for abdominal pain or identified incidentally on imaging studies. Endoscopic ultrasound (EUS) and Endoscopic retrograde cholangiopancreatography (ERCP) are often obtained to establish a diagnosis in these scenarios. However, a significant number of patients still do not have a known underlying cause for CBD dilation. This research aims to uncover the risk factors linked to idiopathic CBD dilation.
Methods: This is a retrospective case-control study of patients with isolated bile duct dilatation who were referred to a tertiary care center for EUS/ERCP. Patients were assigned into two groups according to EUS/ERCP findings, idiopathic CBD dilatation and CBD dilatation with identified etiology. Demographics including age and sex were obtained for each patient. History of cholecystectomy was obtained by reviewing the Imaging study at the time of diagnosis. Patients with chronic narcotic use were identified by the following methods: (1) Prescription for methadone or suboxone (2) Opiate prescription for at least 3 months during the year prior to the ERCP/EUS study. A multiple logistic regression model with a manual selection method of clinically relevant covariates including age > 60, history of cholecystectomy, abnormal total bilirubin, and pancreatic duct dilatation was designed. Sub-group analysis for patients with normal total bilirubin to adjust for confounders.
Results: After the application of selection criteria, 147 were included in the analytic cohort, of whom 68 (46%) patients had idiopathic CBD dilatation. Among patients with identified etiology, hepatobiliary malignancy was diagnosed in 13 (17%) patients and manifested as a suspicious stricture, ampullary or pancreatic lesion. On the other hand, all biopsies obtained in patients with idiopathic CBD dilatation were negative for malignancy. Multivariable logistic regression showed an association between chronic narcotic use aOR 2.8 CI 1.14-6.87 and elevation in total bilirubin aOR 0.3 CI 0.14-0.64 with idiopathic CBD dilatation. The association between Chronic narcotic usage and idiopathic CBD dilatation remained statistically significant aOR 2.92 CI 1.02-8.36 after subgroup analysis for patients with normal total bilirubin (N=78).
Discussion: Abnormal total bilirubin is inversely associated with idiopathic CBD dilatation and Chronic narcotic use is positively associated with idiopathic CBD dilatation even in patients with normal total bilirubin.
Disclosures:
Butros Fakhoury indicated no relevant financial relationships.
Marcel Robles indicated no relevant financial relationships.
Iyiad Alabdul Razzak indicated no relevant financial relationships.
Tiago Barroso Vieira Costa indicated no relevant financial relationships.
Syed Mahmood indicated no relevant financial relationships.
Sandeep Krishnan indicated no relevant financial relationships.
Butros Fakhoury, MD1, Marcel Robles, MD2, Iyiad Alabdul Razzak, MD3, Tiago Barroso Vieira Costa, MD4, Syed K. Mahmood, MD, MPH3, Sandeep Krishnan, MD, PhD3. P2879 - Predictors of Idiopathic Common Bile Duct Dilatation: A Case-Control Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
