Tuesday Poster Session
Category: Biliary/Pancreas
P2886 - Identification of Risk Factors That Worsen Outcomes in Patients With Pancreatic Cancer Undergoing Endoscopic Retrograde Cholangiopancreatography
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- HS
Herman Suga, DO
Jefferson Health
Philadelphia, PA
Presenting Author(s)
Herman Suga, DO1, Jason John, DO2, Chun-Wei Pan, MD3, Kirti Dasu, BA4, Neethi Dasu, DO5, Yaser Khalid, DO6, C. Jonathan Foster, DO7
1Jefferson Health, Philadelphia, PA; 2Jefferson Health, Stratford, NJ; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4Drexel University, Cherry Hill, NJ; 5Jefferson Health, New Jersey, NJ; 6Wright Center for GME/Geisinger Health System, Scranton, PA; 7Jefferson Health, Cherry Hill, NJ
Introduction: Pancreatic cancer is a leading care of morbidity and mortality in the United States. Therapeutic interventions, such as ERCP, play a crucial role in the management of advanced pancreatic cancers. Malignant biliary obstructions from pancreatic cancer have become a common indication for ERCP with balloon dilation or stenting of pancreatic and biliary strictures often being performed. The aim of this study was to identify post-procedural risk factors that lead to worsened in-hospital outcomes of patients with pancreatic cancer undergoing ERCP.
Methods: We identified patients (18 years and older) with and without pancreatic cancer undergoing ERCP from the National Inpatient Sample (NIS) utilizing ICD 10 codes. The NIS, which is a large publicly available all-payer inpatient care database in the USA, was queried from the years 2015-2019. Multivariate regression analysis was used to calculate the odds ratios of in-hospital mortality, the average length of hospital stay (LOS), and hospital charges (TOTHC) using STATA 17 MP.
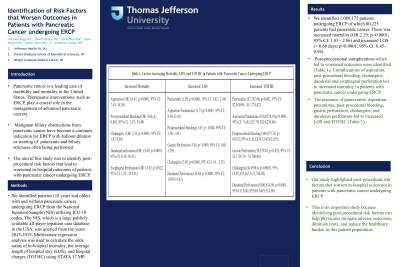
Results: We identified 1,088,175 patients undergoing ERCP of which 80,225 patients had pancreatic cancer. There was increased mortality (OR:2.29; p< 0.0001; 95% CI: 1.83 - 2.86) and increased LOS (+ 0.69 days; p< 0.0001; 95% CI: 0.45- 0.94). Post-processional complications which led to worsened outcomes were identified (Table 1). Complications of aspiration, post-procedural bleeding, cholangitis, and duodenal and esophageal perforation led to increased mortality in patients with pancreatic cancer undergoing ERCP. The presence of pancreatitis, aspiration pneumonia, post-procedural bleeding, gastric perforation, cholangitis, and duodenal perforation led to increased LOS and TOTHC (Table 1).
Discussion: Our study highlighted post-procedural risk factors that worsen in-hospital outcomes in patients with pancreatic cancer undergoing ERCP. This is an important study because identifying post-procedural risk factors can help physicians mitigate adverse outcomes, diminish costs, and reduce the healthcare burden in this patient population.

Disclosures:
Herman Suga, DO1, Jason John, DO2, Chun-Wei Pan, MD3, Kirti Dasu, BA4, Neethi Dasu, DO5, Yaser Khalid, DO6, C. Jonathan Foster, DO7. P2886 - Identification of Risk Factors That Worsen Outcomes in Patients With Pancreatic Cancer Undergoing Endoscopic Retrograde Cholangiopancreatography, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Jefferson Health, Philadelphia, PA; 2Jefferson Health, Stratford, NJ; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4Drexel University, Cherry Hill, NJ; 5Jefferson Health, New Jersey, NJ; 6Wright Center for GME/Geisinger Health System, Scranton, PA; 7Jefferson Health, Cherry Hill, NJ
Introduction: Pancreatic cancer is a leading care of morbidity and mortality in the United States. Therapeutic interventions, such as ERCP, play a crucial role in the management of advanced pancreatic cancers. Malignant biliary obstructions from pancreatic cancer have become a common indication for ERCP with balloon dilation or stenting of pancreatic and biliary strictures often being performed. The aim of this study was to identify post-procedural risk factors that lead to worsened in-hospital outcomes of patients with pancreatic cancer undergoing ERCP.
Methods: We identified patients (18 years and older) with and without pancreatic cancer undergoing ERCP from the National Inpatient Sample (NIS) utilizing ICD 10 codes. The NIS, which is a large publicly available all-payer inpatient care database in the USA, was queried from the years 2015-2019. Multivariate regression analysis was used to calculate the odds ratios of in-hospital mortality, the average length of hospital stay (LOS), and hospital charges (TOTHC) using STATA 17 MP.
Results: We identified 1,088,175 patients undergoing ERCP of which 80,225 patients had pancreatic cancer. There was increased mortality (OR:2.29; p< 0.0001; 95% CI: 1.83 - 2.86) and increased LOS (+ 0.69 days; p< 0.0001; 95% CI: 0.45- 0.94). Post-processional complications which led to worsened outcomes were identified (Table 1). Complications of aspiration, post-procedural bleeding, cholangitis, and duodenal and esophageal perforation led to increased mortality in patients with pancreatic cancer undergoing ERCP. The presence of pancreatitis, aspiration pneumonia, post-procedural bleeding, gastric perforation, cholangitis, and duodenal perforation led to increased LOS and TOTHC (Table 1).
Discussion: Our study highlighted post-procedural risk factors that worsen in-hospital outcomes in patients with pancreatic cancer undergoing ERCP. This is an important study because identifying post-procedural risk factors can help physicians mitigate adverse outcomes, diminish costs, and reduce the healthcare burden in this patient population.

Figure: Table 1
Disclosures:
Herman Suga indicated no relevant financial relationships.
Jason John indicated no relevant financial relationships.
Chun-Wei Pan indicated no relevant financial relationships.
Kirti Dasu indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
Yaser Khalid indicated no relevant financial relationships.
C. Jonathan Foster indicated no relevant financial relationships.
Herman Suga, DO1, Jason John, DO2, Chun-Wei Pan, MD3, Kirti Dasu, BA4, Neethi Dasu, DO5, Yaser Khalid, DO6, C. Jonathan Foster, DO7. P2886 - Identification of Risk Factors That Worsen Outcomes in Patients With Pancreatic Cancer Undergoing Endoscopic Retrograde Cholangiopancreatography, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
