Tuesday Poster Session
Category: Biliary/Pancreas
P2888 - Low Post ERCP Pancreatitis in Safety Net Setting Despite Native Papilla Status: A Dual Center Cross-Sectional Cohort Study
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Patrick Chang, MD
University of Southern California
Los Angeles, California
Presenting Author(s)
Patrick Chang, MD1, James D. Haddad, MD2, Hayley Rogers, MD2, Denis Nguyen, MD3, Maziar Amini, MD4, Jennifer Phan, MD3, Thomas Tielleman, MD2
1University of Southern California, Los Angeles, CA; 2University of Texas Southwestern Medical Center, Dallas, TX; 3Keck School of Medicine of USC, Los Angeles, CA; 4Los Angeles General Hospital, University of Southern California, Los Angeles, CA
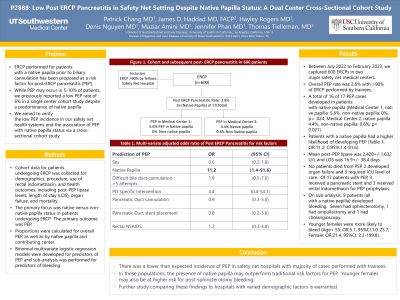
Introduction: ERCP performed for patients with a native papilla prior to biliary cannulation has been proposed as a risk factor for post-ERCP pancreatitis (PEP). While PEP may occur in 5-10% of patients, we previously reported a low PEP rate of 6% in a single center cohort study despite a predominance native papilla. We aimed to verify the low PEP incidence in our safety net health systems and the association of PEP with native papilla status via a cross-sectional cohort study.
Methods: Cohort data for patients undergoing ERCP was collected for demographics, procedure, use of rectal indomethacin, and health outcomes, including post-PEP lipase levels, length of stay (LOS), organ failure, and mortality. The primary focus was native versus non-native papilla status in patients undergoing ERCP. The primary outcome was PEP. Proportions were calculated for overall PEP, as well as by native papilla and contributing center. Binomial multivariate logistic regression models were developed for predictors of PEP and bleeding.
Results: Between July 2022 to February 2023, we captured 600 ERCPs in two major safety net medical centers. Overall PEP rate was 2.8% with >90% of ERCP performed by trainees. A total of 16 of 17 PEP cases developed in patients with native papilla (Medical Center 1, native papilla: 5.6%, non-native papilla: 0%, p= 0.024; Medical Center 2, native papilla: 4.4%, non-native papilla: 0.6%, p= 0.021). Patients with a native papilla had a higher likelihood of developing PEP (Table 1, OR:11.2; CI95%:1.4-91.6).
Mean post-PEP lipase was 2,428+/-1,632 U/L and LOS was 16.9+/- 38.4 days. No patients died from PEP, 2 developed organ failure and 3 required ICU level of care. Of 17 patients with PEP, 3 received a pancreatic stent and 3 received rectal indomethacin for PEP prophylaxis.
On sub-analysis, 9 patients (all with a native papilla) developed bleeding. Seven had sphincterotomy, 1 had ampullectomy and 1 had cholangioscopy. Younger females were more likely to bleed (Age< 55: OR:5.1, 95%CI:1.0-25.7; Female: OR:21.4, 95%CI: 2.3-199.8).
Discussion: We found a significantly lower than expected incidence of PEP in safety net hospitals where the majority of cases were performed with a trainee. In these populations, the presence of native papilla may outperform traditional risk factors for PEP. Younger females may also be at higher risk for post-sphincterotomy bleeding. Further study comparing these findings to hospitals with varied demographic factors is warranted.
Disclosures:
Patrick Chang, MD1, James D. Haddad, MD2, Hayley Rogers, MD2, Denis Nguyen, MD3, Maziar Amini, MD4, Jennifer Phan, MD3, Thomas Tielleman, MD2. P2888 - Low Post ERCP Pancreatitis in Safety Net Setting Despite Native Papilla Status: A Dual Center Cross-Sectional Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Southern California, Los Angeles, CA; 2University of Texas Southwestern Medical Center, Dallas, TX; 3Keck School of Medicine of USC, Los Angeles, CA; 4Los Angeles General Hospital, University of Southern California, Los Angeles, CA
Introduction: ERCP performed for patients with a native papilla prior to biliary cannulation has been proposed as a risk factor for post-ERCP pancreatitis (PEP). While PEP may occur in 5-10% of patients, we previously reported a low PEP rate of 6% in a single center cohort study despite a predominance native papilla. We aimed to verify the low PEP incidence in our safety net health systems and the association of PEP with native papilla status via a cross-sectional cohort study.
Methods: Cohort data for patients undergoing ERCP was collected for demographics, procedure, use of rectal indomethacin, and health outcomes, including post-PEP lipase levels, length of stay (LOS), organ failure, and mortality. The primary focus was native versus non-native papilla status in patients undergoing ERCP. The primary outcome was PEP. Proportions were calculated for overall PEP, as well as by native papilla and contributing center. Binomial multivariate logistic regression models were developed for predictors of PEP and bleeding.
Results: Between July 2022 to February 2023, we captured 600 ERCPs in two major safety net medical centers. Overall PEP rate was 2.8% with >90% of ERCP performed by trainees. A total of 16 of 17 PEP cases developed in patients with native papilla (Medical Center 1, native papilla: 5.6%, non-native papilla: 0%, p= 0.024; Medical Center 2, native papilla: 4.4%, non-native papilla: 0.6%, p= 0.021). Patients with a native papilla had a higher likelihood of developing PEP (Table 1, OR:11.2; CI95%:1.4-91.6).
Mean post-PEP lipase was 2,428+/-1,632 U/L and LOS was 16.9+/- 38.4 days. No patients died from PEP, 2 developed organ failure and 3 required ICU level of care. Of 17 patients with PEP, 3 received a pancreatic stent and 3 received rectal indomethacin for PEP prophylaxis.
On sub-analysis, 9 patients (all with a native papilla) developed bleeding. Seven had sphincterotomy, 1 had ampullectomy and 1 had cholangioscopy. Younger females were more likely to bleed (Age< 55: OR:5.1, 95%CI:1.0-25.7; Female: OR:21.4, 95%CI: 2.3-199.8).
Discussion: We found a significantly lower than expected incidence of PEP in safety net hospitals where the majority of cases were performed with a trainee. In these populations, the presence of native papilla may outperform traditional risk factors for PEP. Younger females may also be at higher risk for post-sphincterotomy bleeding. Further study comparing these findings to hospitals with varied demographic factors is warranted.
Disclosures:
Patrick Chang indicated no relevant financial relationships.
James Haddad indicated no relevant financial relationships.
Hayley Rogers indicated no relevant financial relationships.
Denis Nguyen indicated no relevant financial relationships.
Maziar Amini indicated no relevant financial relationships.
Jennifer Phan: Boston Scientific – Consultant. Cook Medical – Consultant. Olympus – Consultant.
Thomas Tielleman indicated no relevant financial relationships.
Patrick Chang, MD1, James D. Haddad, MD2, Hayley Rogers, MD2, Denis Nguyen, MD3, Maziar Amini, MD4, Jennifer Phan, MD3, Thomas Tielleman, MD2. P2888 - Low Post ERCP Pancreatitis in Safety Net Setting Despite Native Papilla Status: A Dual Center Cross-Sectional Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
