Tuesday Poster Session
Category: Liver
P3891 - A Twisted Fate: Unraveling the Enigma of Portal Vein Thrombosis in Hepatic Adenomas
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- AZ
Anas Zaher, MD
New York Presbyterian Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Anas Zaher, MD1, Harsh Patel, MD1, Megha Reddy, MD1, Pratishtha Singh, MD2, Meghaben Kothari, MD1
1New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Hepatocellular adenomas (HCAs) are rare benign liver tumors affecting 3 to 4 per 100,000 individuals. Their development is primarily driven by sex, hormones and genetic predisposition. They can be asymptomatic or present as life threatening intra-abdominal bleeding. Prompt diagnosis and intervention are crucial to prevent morbidity and mortality associated with rupture and bleed. We present a case of HCA with rupture in an 80-year-old male.
Case Description/Methods: An 80-year-old male with a history of portal vein thrombosis (PVT) on warfarin for 40 years presented to the ER with severe sudden cramping right sided abdominal pain. Vitals were remarkable for hypotension to 63/48 mmHg with tachycardia. Physical exam was significant for jaundice with scleral icterus and right upper quadrant abdominal tenderness associated with guarding. Laboratory tests are shown in the table.
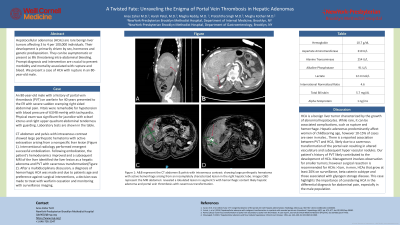
CT abdomen and pelvis with intravenous contrast showed large perihepatic hematoma with active extravasation arising from a nonspecific liver lesion (Figure 1). Interventional radiology performed emergent successful embolization. Following embolization, the patient's hemodynamics improved and a subsequent MRI of the liver identified the liver lesion as a hepatic adenoma and PVT with cavernous transformation(Figure 2). After a multidisciplinary discussion, a diagnosis of hemorrhagic HCA was made and due to the patient's age and preference against surgical interventions, a decision was made to treat with warfarin cessation and monitoring with surveillance imaging.
Discussion: HCA is a benign liver tumor characterized by the growth of abnormal hepatocytes. While rare, it can be associated with complications, such as rupture and hemorrhage. Hepatic adenomas predominantly affect women of childbearing age, however, 10-15% of cases are seen in males. There is a reported association between PVT and HCA, likely due to a cavernous transformation of the portal vein resulting in altered vasculature and subsequent hypervascular nodules. Our patient's history of PVT likely contributed to the development of HCA. Management involves observation for smaller tumors; however surgical resection is recommended for HCAs >5cm, in men, HCAs that grow at least 20% on surveillance, beta-catenin subtype and those associated with glycogen storage disease. This case highlights the importance of considering HCA in the differential diagnosis of abdominal pain, especially in the male population.

Disclosures:
Anas Zaher, MD1, Harsh Patel, MD1, Megha Reddy, MD1, Pratishtha Singh, MD2, Meghaben Kothari, MD1. P3891 - A Twisted Fate: Unraveling the Enigma of Portal Vein Thrombosis in Hepatic Adenomas, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Hepatocellular adenomas (HCAs) are rare benign liver tumors affecting 3 to 4 per 100,000 individuals. Their development is primarily driven by sex, hormones and genetic predisposition. They can be asymptomatic or present as life threatening intra-abdominal bleeding. Prompt diagnosis and intervention are crucial to prevent morbidity and mortality associated with rupture and bleed. We present a case of HCA with rupture in an 80-year-old male.
Case Description/Methods: An 80-year-old male with a history of portal vein thrombosis (PVT) on warfarin for 40 years presented to the ER with severe sudden cramping right sided abdominal pain. Vitals were remarkable for hypotension to 63/48 mmHg with tachycardia. Physical exam was significant for jaundice with scleral icterus and right upper quadrant abdominal tenderness associated with guarding. Laboratory tests are shown in the table.
CT abdomen and pelvis with intravenous contrast showed large perihepatic hematoma with active extravasation arising from a nonspecific liver lesion (Figure 1). Interventional radiology performed emergent successful embolization. Following embolization, the patient's hemodynamics improved and a subsequent MRI of the liver identified the liver lesion as a hepatic adenoma and PVT with cavernous transformation(Figure 2). After a multidisciplinary discussion, a diagnosis of hemorrhagic HCA was made and due to the patient's age and preference against surgical interventions, a decision was made to treat with warfarin cessation and monitoring with surveillance imaging.
Discussion: HCA is a benign liver tumor characterized by the growth of abnormal hepatocytes. While rare, it can be associated with complications, such as rupture and hemorrhage. Hepatic adenomas predominantly affect women of childbearing age, however, 10-15% of cases are seen in males. There is a reported association between PVT and HCA, likely due to a cavernous transformation of the portal vein resulting in altered vasculature and subsequent hypervascular nodules. Our patient's history of PVT likely contributed to the development of HCA. Management involves observation for smaller tumors; however surgical resection is recommended for HCAs >5cm, in men, HCAs that grow at least 20% on surveillance, beta-catenin subtype and those associated with glycogen storage disease. This case highlights the importance of considering HCA in the differential diagnosis of abdominal pain, especially in the male population.

Figure: *Figure 1: A&B represents the CT abdomen & pelvis with intravenous contrast: showing a large perihepatic hematoma with active hemorrhage arising from an incompletely characterized lesion in the right hepatic lobe.
*Figure 2 C&D represents the MRI abdomen: revealed a lobulated lesion in segment 5 with hemorrhagic content likely hepatic adenoma and portal vein thrombosis with cavernous transformation.
*Figure 2 C&D represents the MRI abdomen: revealed a lobulated lesion in segment 5 with hemorrhagic content likely hepatic adenoma and portal vein thrombosis with cavernous transformation.
Disclosures:
Anas Zaher indicated no relevant financial relationships.
Harsh Patel indicated no relevant financial relationships.
Megha Reddy indicated no relevant financial relationships.
Pratishtha Singh indicated no relevant financial relationships.
Meghaben Kothari indicated no relevant financial relationships.
Anas Zaher, MD1, Harsh Patel, MD1, Megha Reddy, MD1, Pratishtha Singh, MD2, Meghaben Kothari, MD1. P3891 - A Twisted Fate: Unraveling the Enigma of Portal Vein Thrombosis in Hepatic Adenomas, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
