Tuesday Poster Session
Category: Liver
P3913 - Dire Consequences of Superimposed Infection of a Simple Hepatic Cyst
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Tahminah Kausar, MD
Reading Hospital Tower Health
Reading, PA
Presenting Author(s)
Tahminah Kausar, MD1, Sara Khan, MD2, Shefali Amin, DO, MSEd3, Jakob Nypaver, 2, Alexis Seery, 2, Abhishek hariharan, MD2, Erik Wolters, DO2
1Reading Hospital Tower Health, Reading, PA; 2Tower Health-Reading Hospital, Reading, PA; 3Reading Hospital, Reading, PA
Introduction: Simple Hepatic Cysts (SHC) in the liver are typically asymptomatic, benign, and tend to have a female predominance due to the role of estrogen in their development. They are often an incidental finding on imaging, having a prevalence of around 18%. Infectious hepatic cysts that arise from secondary infection of SHCs are a rare but serious sequelae.
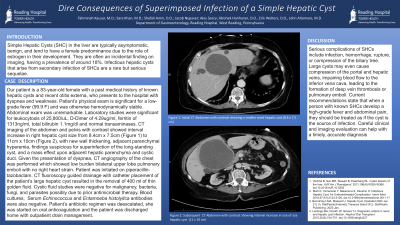
Case Description/Methods: Our patient is a 83-year-old female with a past medical history of known hepatic cysts and recent otitis externa, who presents to the hospital with dyspnea and weakness. Patient’s physical exam is significant for a low grade fever (99.9 F), and was otherwise hemodynamically stable. Abdominal exam was unremarkable. Laboratory studies were significant for leukocytosis of 25,800/uL, D-Dimer of 4.29ug/ml, ferritin of 1313ng/ml, total bilirubin 1.1mg/dl and normal transaminases. CT imaging of the abdomen and pelvis with contrast showed interval increase in right hepatic cyst size from 8.4cm x 7.5cm to 11cm x 10cm, with new wall thickening, adjacent parenchymal hyperemia, findings suspicious for superinfection of the long standing cyst, and a mass effect upon adjacent hepatic parenchyma and cystic duct. Given the presentation of dyspnea, CT angiography of the chest was performed which showed low burden bilateral upper lobe pulmonary emboli with no right heart strain. Patient was initiated on piperacillin-tazobactam. CT fluoroscopy guided drainage with catheter placement of the patient’s large hepatic cyst resulted in the removal of 400 ml of thin golden fluid. Cystic fluid studies were negative for malignancy, bacteria, fungi, and parasites possibly due to prior antimicrobial therapy. Blood cultures, Serum Echinococcus and Entamoeba histolyitca antibodies were also negative. Patient’s antibiotic regimen was deescalated, she was started on oral anticoagulation and the patient was discharged home with outpatient drain management.
Discussion: Serious complications of SHCs include infection, hemorrhage, rupture, or compression of the biliary tree. Large cysts may even cause compression of the portal and hepatic veins, impairing blood flow to the inferior vena cava, leading to the formation of deep vein thrombosis or pulmonary emboli. Current recommendations state that when a person with known SHCs develop a high-grade fever and abdominal pain, they should be treated as if the cyst is the source of infection. Careful clinical and imaging evaluation can help with a timely, accurate diagnosis.

Disclosures:
Tahminah Kausar, MD1, Sara Khan, MD2, Shefali Amin, DO, MSEd3, Jakob Nypaver, 2, Alexis Seery, 2, Abhishek hariharan, MD2, Erik Wolters, DO2. P3913 - Dire Consequences of Superimposed Infection of a Simple Hepatic Cyst, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Reading Hospital Tower Health, Reading, PA; 2Tower Health-Reading Hospital, Reading, PA; 3Reading Hospital, Reading, PA
Introduction: Simple Hepatic Cysts (SHC) in the liver are typically asymptomatic, benign, and tend to have a female predominance due to the role of estrogen in their development. They are often an incidental finding on imaging, having a prevalence of around 18%. Infectious hepatic cysts that arise from secondary infection of SHCs are a rare but serious sequelae.
Case Description/Methods: Our patient is a 83-year-old female with a past medical history of known hepatic cysts and recent otitis externa, who presents to the hospital with dyspnea and weakness. Patient’s physical exam is significant for a low grade fever (99.9 F), and was otherwise hemodynamically stable. Abdominal exam was unremarkable. Laboratory studies were significant for leukocytosis of 25,800/uL, D-Dimer of 4.29ug/ml, ferritin of 1313ng/ml, total bilirubin 1.1mg/dl and normal transaminases. CT imaging of the abdomen and pelvis with contrast showed interval increase in right hepatic cyst size from 8.4cm x 7.5cm to 11cm x 10cm, with new wall thickening, adjacent parenchymal hyperemia, findings suspicious for superinfection of the long standing cyst, and a mass effect upon adjacent hepatic parenchyma and cystic duct. Given the presentation of dyspnea, CT angiography of the chest was performed which showed low burden bilateral upper lobe pulmonary emboli with no right heart strain. Patient was initiated on piperacillin-tazobactam. CT fluoroscopy guided drainage with catheter placement of the patient’s large hepatic cyst resulted in the removal of 400 ml of thin golden fluid. Cystic fluid studies were negative for malignancy, bacteria, fungi, and parasites possibly due to prior antimicrobial therapy. Blood cultures, Serum Echinococcus and Entamoeba histolyitca antibodies were also negative. Patient’s antibiotic regimen was deescalated, she was started on oral anticoagulation and the patient was discharged home with outpatient drain management.
Discussion: Serious complications of SHCs include infection, hemorrhage, rupture, or compression of the biliary tree. Large cysts may even cause compression of the portal and hepatic veins, impairing blood flow to the inferior vena cava, leading to the formation of deep vein thrombosis or pulmonary emboli. Current recommendations state that when a person with known SHCs develop a high-grade fever and abdominal pain, they should be treated as if the cyst is the source of infection. Careful clinical and imaging evaluation can help with a timely, accurate diagnosis.

Figure: CT Abdomen and Pelvis with contrast showing enlarged hepatic cyst
Disclosures:
Tahminah Kausar indicated no relevant financial relationships.
Sara Khan indicated no relevant financial relationships.
Shefali Amin indicated no relevant financial relationships.
Jakob Nypaver indicated no relevant financial relationships.
Alexis Seery indicated no relevant financial relationships.
Abhishek hariharan indicated no relevant financial relationships.
Erik Wolters indicated no relevant financial relationships.
Tahminah Kausar, MD1, Sara Khan, MD2, Shefali Amin, DO, MSEd3, Jakob Nypaver, 2, Alexis Seery, 2, Abhishek hariharan, MD2, Erik Wolters, DO2. P3913 - Dire Consequences of Superimposed Infection of a Simple Hepatic Cyst, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
