Tuesday Poster Session
Category: Liver
P3920 - Elevated Liver Enzymes: Is Phenytoin the Culprit?
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpeg.jpg)
Daniyal Raza, MD
LSU Health Sciences Center
Shreveport, LA
Presenting Author(s)
Vatsa Bhavsar, MBBS1, Poojan Prajapati, MBBS2, Daniyal Raza, MD3, Syed Musa Raza, MD3, Hassaan A. Zia, MD3
1B.J. Medical College, Shreveport, LA; 2B.J. Medical College, Ahmedabad, Gujarat, India; 3LSU Health Sciences Center, Shreveport, LA
Introduction: Drug-induced hepatotoxicity is difficult to diagnose as it is similar to other hepatobiliary disorders, and it can cause acute or chronic liver injury. Phenytoin, an effective anticonvulsant, is rare but known cause of acute idiosyncratic drug-induced liver disease, which can be fatal. Most cases of phenytoin-induced liver injury result from a hypersensitivity reaction resembling immuno-allergic hepatotoxicity. Here, we present a rare case of phenytoin-induced hepatotoxicity.
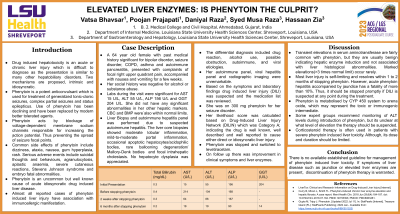
Case Description/Methods: A 64-year-old female with history of bipolar disorder, seizure disorder (on phenytoin), and autoimmune pancreatitis presented with right upper quadrant pain, nausea, and vomiting. Patient denied alcohol or drug use. Lab results showed elevated AST (15 U/L), ALT (55 U/L), ALP (156 U/L), and GGT (204 U/L), other hepatic markers were within normal limits. Platelet count and INR were within normal limit. Autoimmune panel, viral hepatitis panel, and radiographic imaging were unremarkable. Liver core biopsies showed moderate lobular inflammation, mild portal inflammation, few apoptotic hepatocytes, rare Mallory-Denk bodies, and focal intrahepatic cholestasis. Possible causes were drug reaction, alcohol use, obstruction, autoimmune, and viral etiologies. Drug-induced liver injury was suspected, and drug list was reviewed. Likelihood score, based on Drug-Induced Liver Injury Network (DILIN), classified drug as Category A, indicating a well-known association with liver injury. Phenytoin was discontinued and replaced with levetiracetam. Follow-up revealed improvement in symptoms and liver enzymes.
Discussion: Transient elevation in serum aminotransferase is common with phenytoin, usually indicating hepatic enzyme induction without histological abnormalities. Significant elevation beyond three times standard limit is rare. Most liver injuries from phenytoin are self-limiting and resolve within few months after discontinuation. However, acute phenytoin hepatitis with jaundice can be fatal, with a fatality rate over 10%. Thus, immediate discontinuation of phenytoin is advised if drug-induced liver injury (DILI) is suspected. While monitoring ALT levels is recommended, there is no clear threshold for discontinuing therapy based on ALT elevation. In severe cases of phenytoin-induced liver toxicity, corticosteroid therapy may be used cautiously and in minimal doses. There are no established guidelines, but discontinuing phenytoin therapy is warranted if liver disease symptoms or elevated liver enzymes are present.
Disclosures:
Vatsa Bhavsar, MBBS1, Poojan Prajapati, MBBS2, Daniyal Raza, MD3, Syed Musa Raza, MD3, Hassaan A. Zia, MD3. P3920 - Elevated Liver Enzymes: Is Phenytoin the Culprit?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1B.J. Medical College, Shreveport, LA; 2B.J. Medical College, Ahmedabad, Gujarat, India; 3LSU Health Sciences Center, Shreveport, LA
Introduction: Drug-induced hepatotoxicity is difficult to diagnose as it is similar to other hepatobiliary disorders, and it can cause acute or chronic liver injury. Phenytoin, an effective anticonvulsant, is rare but known cause of acute idiosyncratic drug-induced liver disease, which can be fatal. Most cases of phenytoin-induced liver injury result from a hypersensitivity reaction resembling immuno-allergic hepatotoxicity. Here, we present a rare case of phenytoin-induced hepatotoxicity.
Case Description/Methods: A 64-year-old female with history of bipolar disorder, seizure disorder (on phenytoin), and autoimmune pancreatitis presented with right upper quadrant pain, nausea, and vomiting. Patient denied alcohol or drug use. Lab results showed elevated AST (15 U/L), ALT (55 U/L), ALP (156 U/L), and GGT (204 U/L), other hepatic markers were within normal limits. Platelet count and INR were within normal limit. Autoimmune panel, viral hepatitis panel, and radiographic imaging were unremarkable. Liver core biopsies showed moderate lobular inflammation, mild portal inflammation, few apoptotic hepatocytes, rare Mallory-Denk bodies, and focal intrahepatic cholestasis. Possible causes were drug reaction, alcohol use, obstruction, autoimmune, and viral etiologies. Drug-induced liver injury was suspected, and drug list was reviewed. Likelihood score, based on Drug-Induced Liver Injury Network (DILIN), classified drug as Category A, indicating a well-known association with liver injury. Phenytoin was discontinued and replaced with levetiracetam. Follow-up revealed improvement in symptoms and liver enzymes.
Discussion: Transient elevation in serum aminotransferase is common with phenytoin, usually indicating hepatic enzyme induction without histological abnormalities. Significant elevation beyond three times standard limit is rare. Most liver injuries from phenytoin are self-limiting and resolve within few months after discontinuation. However, acute phenytoin hepatitis with jaundice can be fatal, with a fatality rate over 10%. Thus, immediate discontinuation of phenytoin is advised if drug-induced liver injury (DILI) is suspected. While monitoring ALT levels is recommended, there is no clear threshold for discontinuing therapy based on ALT elevation. In severe cases of phenytoin-induced liver toxicity, corticosteroid therapy may be used cautiously and in minimal doses. There are no established guidelines, but discontinuing phenytoin therapy is warranted if liver disease symptoms or elevated liver enzymes are present.
Disclosures:
Vatsa Bhavsar indicated no relevant financial relationships.
Poojan Prajapati indicated no relevant financial relationships.
Daniyal Raza indicated no relevant financial relationships.
Syed Musa Raza indicated no relevant financial relationships.
Hassaan A. Zia indicated no relevant financial relationships.
Vatsa Bhavsar, MBBS1, Poojan Prajapati, MBBS2, Daniyal Raza, MD3, Syed Musa Raza, MD3, Hassaan A. Zia, MD3. P3920 - Elevated Liver Enzymes: Is Phenytoin the Culprit?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
