Tuesday Poster Session
Category: Liver
P3921 - Acute Liver Injury or Acute Liver Failure? A Unique Presentation of Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Michal Wiseman, MD
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Michal Wiseman, MD1, Kelvin Liao, MD2, Trevor J. Mathias, PhD2, Stephen Schwartz, DO3, Neha Jakhete, MD1
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD; 3University of Maryland Medical System, Baltimore, MD
Introduction: Acute liver failure (ALF) is defined by liver injury causing synthetic dysfunction (coagulopathy) and encephalopathy within 26 weeks from insult in patients without preexisting liver disease. ALF must be distinguished from acute liver injury—which does not exhibit encephalopathy—due to the difference in management and potential need for liver transplant (LT) in ALF. We present a case of acute liver injury with concern for ALF caused by congestive hepatopathy due to chronic thromboembolic pulmonary hypertension (CTEPH).
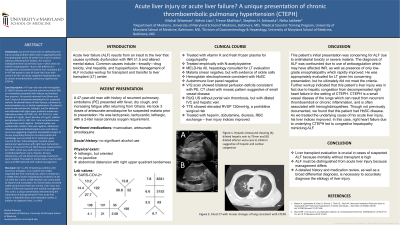
Case Description/Methods: A 47-year-old man with Hemoglobin SC (HbSC) disease and recurrent pulmonary emboli (PE) on rivaroxaban presented with malaise and elevated liver enzymes. He recently returned from Ghana and took 3 doses of artesunate-amodiaquine for suspected malaria. He denied history of liver disease, substance or acetaminophen use, or herbal supplements. On physical exam he was tachycardic, lethargic, and his abdomen was distended with right upper quadrant tenderness. Laboratory values: AST 8331 U/L, ALT 3152 U/L, total bilirubin 6.7 mg/dL, direct bilirubin 4.0 mg/dL, alkaline phosphatase 63 U/L, INR 13.8. Viral and autoimmune hepatitis labs were negative. Acetaminophen level was undetectable. Malaria stain was negative. Abdominal ultrasound showed dilated hepatic veins and inferior vena cava suggesting congestive hepatopathy (Figure 1). He was empirically started on N-acetylcysteine and hepatology was consulted for LT evaluation given concern for ALF. Echocardiogram revealed severe pulmonary hypertension with right heart dysfunction. History of recurrent PE and HbSC disease raised concern for CTEPH, which was confirmed on CT chest and ventilation/perfusion scans. Heparin, diuresis, dobutamine, and red blood cell exchange transfusion were initiated. The patient's mental status, liver function tests, and INR improved with medical management.
Discussion: ALF is a life-threatening condition with numerous etiologies. In our patient we initially suspected ALF from antimalarials, which is related to a 1:15000 rate of severe hepatotoxicity. However, he did not meet ALF criteria as INR elevation was confounded by heparin and rivaroxaban. His mental status remained stable and ammonia level was normal. Liver injury was due to CTEPH and improved with medical management. This case is a unique presentation demonstrating the importance of distinguishing ALF from acute liver injury—a detailed history and medication review, in addition to diagnostic tests, is critical.

Disclosures:
Michal Wiseman, MD1, Kelvin Liao, MD2, Trevor J. Mathias, PhD2, Stephen Schwartz, DO3, Neha Jakhete, MD1. P3921 - Acute Liver Injury or Acute Liver Failure? A Unique Presentation of Chronic Thromboembolic Pulmonary Hypertension (CTEPH), ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD; 3University of Maryland Medical System, Baltimore, MD
Introduction: Acute liver failure (ALF) is defined by liver injury causing synthetic dysfunction (coagulopathy) and encephalopathy within 26 weeks from insult in patients without preexisting liver disease. ALF must be distinguished from acute liver injury—which does not exhibit encephalopathy—due to the difference in management and potential need for liver transplant (LT) in ALF. We present a case of acute liver injury with concern for ALF caused by congestive hepatopathy due to chronic thromboembolic pulmonary hypertension (CTEPH).
Case Description/Methods: A 47-year-old man with Hemoglobin SC (HbSC) disease and recurrent pulmonary emboli (PE) on rivaroxaban presented with malaise and elevated liver enzymes. He recently returned from Ghana and took 3 doses of artesunate-amodiaquine for suspected malaria. He denied history of liver disease, substance or acetaminophen use, or herbal supplements. On physical exam he was tachycardic, lethargic, and his abdomen was distended with right upper quadrant tenderness. Laboratory values: AST 8331 U/L, ALT 3152 U/L, total bilirubin 6.7 mg/dL, direct bilirubin 4.0 mg/dL, alkaline phosphatase 63 U/L, INR 13.8. Viral and autoimmune hepatitis labs were negative. Acetaminophen level was undetectable. Malaria stain was negative. Abdominal ultrasound showed dilated hepatic veins and inferior vena cava suggesting congestive hepatopathy (Figure 1). He was empirically started on N-acetylcysteine and hepatology was consulted for LT evaluation given concern for ALF. Echocardiogram revealed severe pulmonary hypertension with right heart dysfunction. History of recurrent PE and HbSC disease raised concern for CTEPH, which was confirmed on CT chest and ventilation/perfusion scans. Heparin, diuresis, dobutamine, and red blood cell exchange transfusion were initiated. The patient's mental status, liver function tests, and INR improved with medical management.
Discussion: ALF is a life-threatening condition with numerous etiologies. In our patient we initially suspected ALF from antimalarials, which is related to a 1:15000 rate of severe hepatotoxicity. However, he did not meet ALF criteria as INR elevation was confounded by heparin and rivaroxaban. His mental status remained stable and ammonia level was normal. Liver injury was due to CTEPH and improved with medical management. This case is a unique presentation demonstrating the importance of distinguishing ALF from acute liver injury—a detailed history and medication review, in addition to diagnostic tests, is critical.

Figure: Hepatic ultrasound showing (A) dilated hepatic vein to 75mm and (B) dilated inferior vena cava to 244mm suggestive of hepatic and cardiac congestion
Disclosures:
Michal Wiseman indicated no relevant financial relationships.
Kelvin Liao indicated no relevant financial relationships.
Trevor Mathias indicated no relevant financial relationships.
Stephen Schwartz indicated no relevant financial relationships.
Neha Jakhete indicated no relevant financial relationships.
Michal Wiseman, MD1, Kelvin Liao, MD2, Trevor J. Mathias, PhD2, Stephen Schwartz, DO3, Neha Jakhete, MD1. P3921 - Acute Liver Injury or Acute Liver Failure? A Unique Presentation of Chronic Thromboembolic Pulmonary Hypertension (CTEPH), ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
