Tuesday Poster Session
Category: Liver
P3922 - Current Guidelines for Hepatocellular Carcinoma Screening Could Potentially Miss Advanced Cases: Case Report and Literature Review
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- KA
Kian Abdul-Baki, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Kian Abdul-Baki, DO1, Raakhi Menon, DO1, Kanana Aburayyan, MD1, Peter Young, MD2, Akshata Moghe, MD, PhD2
1University of Texas Medical Branch, Galveston, TX; 2UTMB, Galveston, TX
Introduction: Hepatocellular carcinoma (HCC) is the most common primary liver malignancy. Approximately 80% of patients with HCC have underlying cirrhosis. Current guidelines recommend HCC screening for cirrhotic patients every 6 months with right upper quadrant ultrasound (RUQ US) with or without alpha-fetoprotein (AFP). We present a patient with elevated AFP and advanced HCC which was not seen on right upper quadrant ultrasound (RUQ US).
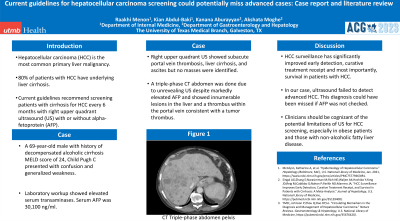
Case Description/Methods: A 69-year-old non-obese male with decompensated alcohol-related cirrhosis (MELD-Na 24, Child Pugh C) presented with confusion and generalized weakness. Vital signs were stable. Labs were as follows: INR 1.8, total bilirubin 7.9, platelets 227, albumin 2.9, Alkaline phosphatase 199, ALT 40, AST 139, and serum AFP was 30,100 ng/ml. RUQ US showed subacute portal vein thrombosis, liver cirrhosis, and moderate ascites but no masses were identified. A triple-phase CT abdomen/pelvis (AP) was obtained given markedly elevated AFP and showed expansile enhancing tumor thrombus (LR-Tumor in vein) within the main portal vein and intrahepatic portal venous branches, a large heterogeneously hypoenhancing lesion in segment VII of the right liver with an apparent capsule measuring 5.8 cm, (LI-RADS 4), and innumerable additional hypoenhancing lesions throughout both lobes of the liver measuring up to 3.8 cm (at least LI-RADS 3). Imaging also showed lytic lesions in multiple vertebral bodies suggestive of osseous metastatic disease. Oncology was consulted and deemed the patient was not a candidate for systemic therapy given metastatic disease in the setting of severely decompensated cirrhosis. Goals of care were discussed, and he was subsequently transitioned to hospice care.
Discussion: HCC surveillance significantly improves early detection, curative treatment receipt, and most importantly, survival in patients with HCC. In our case, RUQ US failed to detect advanced HCC. This diagnosis could have been missed if AFP was not checked. AFP alone has a 63% sensitivity and 88.7% specificity for the detection of HCC. Whereas, US has a sensitivity of 45.7% and a specificity of 100%. The combination of US and AFP has a sensitivity of 97% and specificity of 87.3%. Current guidelines do not mandate checking AFP as part of HCC screening, but we believe this could be advantageous given the limitations of US, particularly in obese patients and those with non-alcoholic fatty liver disease as the sensitivity of US is known to be lower in these patient populations.

Disclosures:
Kian Abdul-Baki, DO1, Raakhi Menon, DO1, Kanana Aburayyan, MD1, Peter Young, MD2, Akshata Moghe, MD, PhD2. P3922 - Current Guidelines for Hepatocellular Carcinoma Screening Could Potentially Miss Advanced Cases: Case Report and Literature Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2UTMB, Galveston, TX
Introduction: Hepatocellular carcinoma (HCC) is the most common primary liver malignancy. Approximately 80% of patients with HCC have underlying cirrhosis. Current guidelines recommend HCC screening for cirrhotic patients every 6 months with right upper quadrant ultrasound (RUQ US) with or without alpha-fetoprotein (AFP). We present a patient with elevated AFP and advanced HCC which was not seen on right upper quadrant ultrasound (RUQ US).
Case Description/Methods: A 69-year-old non-obese male with decompensated alcohol-related cirrhosis (MELD-Na 24, Child Pugh C) presented with confusion and generalized weakness. Vital signs were stable. Labs were as follows: INR 1.8, total bilirubin 7.9, platelets 227, albumin 2.9, Alkaline phosphatase 199, ALT 40, AST 139, and serum AFP was 30,100 ng/ml. RUQ US showed subacute portal vein thrombosis, liver cirrhosis, and moderate ascites but no masses were identified. A triple-phase CT abdomen/pelvis (AP) was obtained given markedly elevated AFP and showed expansile enhancing tumor thrombus (LR-Tumor in vein) within the main portal vein and intrahepatic portal venous branches, a large heterogeneously hypoenhancing lesion in segment VII of the right liver with an apparent capsule measuring 5.8 cm, (LI-RADS 4), and innumerable additional hypoenhancing lesions throughout both lobes of the liver measuring up to 3.8 cm (at least LI-RADS 3). Imaging also showed lytic lesions in multiple vertebral bodies suggestive of osseous metastatic disease. Oncology was consulted and deemed the patient was not a candidate for systemic therapy given metastatic disease in the setting of severely decompensated cirrhosis. Goals of care were discussed, and he was subsequently transitioned to hospice care.
Discussion: HCC surveillance significantly improves early detection, curative treatment receipt, and most importantly, survival in patients with HCC. In our case, RUQ US failed to detect advanced HCC. This diagnosis could have been missed if AFP was not checked. AFP alone has a 63% sensitivity and 88.7% specificity for the detection of HCC. Whereas, US has a sensitivity of 45.7% and a specificity of 100%. The combination of US and AFP has a sensitivity of 97% and specificity of 87.3%. Current guidelines do not mandate checking AFP as part of HCC screening, but we believe this could be advantageous given the limitations of US, particularly in obese patients and those with non-alcoholic fatty liver disease as the sensitivity of US is known to be lower in these patient populations.

Figure: A & B) Ultrasonography of the right and left hepatic lobes demonstrates surface nodularity, coarsened echotexture and diffusely heterogenous hepatic echogenicity.
C & D) Contrast-enhanced CT of the abdomen demonstrates an observation in segment VIII measuring up to 5.8 cm with a subtle enhancing capsule. No definite washout or arterial non-peripheral hyperenhancement is definitely seen, LR-4. Numerous additional LR-3 observations are also seen. Cirrhotic liver morphology and portomesenteric venous thrombi are present.
C & D) Contrast-enhanced CT of the abdomen demonstrates an observation in segment VIII measuring up to 5.8 cm with a subtle enhancing capsule. No definite washout or arterial non-peripheral hyperenhancement is definitely seen, LR-4. Numerous additional LR-3 observations are also seen. Cirrhotic liver morphology and portomesenteric venous thrombi are present.
Disclosures:
Kian Abdul-Baki indicated no relevant financial relationships.
Raakhi Menon indicated no relevant financial relationships.
Kanana Aburayyan indicated no relevant financial relationships.
Peter Young indicated no relevant financial relationships.
Akshata Moghe indicated no relevant financial relationships.
Kian Abdul-Baki, DO1, Raakhi Menon, DO1, Kanana Aburayyan, MD1, Peter Young, MD2, Akshata Moghe, MD, PhD2. P3922 - Current Guidelines for Hepatocellular Carcinoma Screening Could Potentially Miss Advanced Cases: Case Report and Literature Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
