Tuesday Poster Session
Category: Biliary/Pancreas
P2928 - Pancreatic Tuberculosis with Suspected Duodenal Fistula in an Immunocompromised Patient
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Duha Zaffar, MBBS, MD
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Duha Zaffar, MBBS, MD1, Chet Bahadur. Ranabhat, MBBS, MD2, Abdellatif Ismail, MBBS, MD2, Gurdeep Gogna, MD3, Gracia Viana. Rodriguez, MBBS, MD, DM4, Disha Sharma, MBBS5, Raymond Kim, MD, DM4
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Maryland Medical Center Midtown Campus, Baltimore, MD; 3American University of Antigua, Baltimore, MD; 4University of Maryland Medical Center, Baltimore, MD; 5University of Maryland, Baltimore, MD
Introduction: Pancreatic Tuberculosis (TB) is rare, likely due to the effect of pancreatic enzymes that confer protection against mycobacterium tuberculosis (MTB)¹·². However, suspicion should be high in those with pancreatic lesions and history of HIV, organ transplant or relevant immigration history. Our patient had pancreatic tuberculosis with suspected duodenal fistula with complete resolution of symptoms and the fistulous tract with a reduction of the size of the pancreatic lesion on imaging after 1 month of anti-tubercular therapy (ATT).
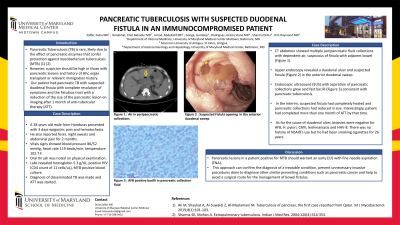
Case Description/Methods: A 38 years old male from Honduras presented with 3 days epigastric pain and hematochezia. He also reported fever, night sweats and abdominal pain for 2 months. Vitals signs showed blood pressure 86/52 mmHg, heart rate 119 beats/min, temperature 102.7 F. Oral thrush was noted on physical examination. Labs revealed hemoglobin 5.3 g/dL, positive HIV (CD4 count of 11 cells/uL), MTB positive blood culture. Diagnosis of disseminated TB was made and ATT was started. Computed Tomography (CT) abdomen showed multiple peripancreatic fluid collections with dependent air, suspicious of fistula with adjacent bowel (Figure 1). Upper endoscopy revealed a duodenal ulcer and suspected fistula (Figure 2) in the anterior duodenal sweep. Endoscopic ultrasound (EUS) with aspiration of pancreatic collections grew acid fast bacilli (Figure 3) consistent with pancreatic tuberculosis. In the interim, suspected fistula had completely healed and pancreatic collections had reduced in size. Interestingly, patient had completed more than one month of ATT by that time. As for the cause of duodenal ulcer, biopsies were negative for AFB, helicobacter pylori, cytomegalovirus, leishmaniasis and human herpes virus-8. There was no history of NSAID’s use but he had been smoking cigarettes for 26 years.
Discussion: Pancreatic lesions in a patient positive for MTB should warrant an early EUS with fine needle aspiration (FNA). This approach can confirm the diagnosis of a treatable condition, prevent unnecessary invasive procedures done to diagnose other similar presenting conditions such as pancreatic cancer and also help to avoid a surgical route for the management of bowel fistulas.
1) Ali M, Shaukat A, Al-Suwaidi Z, Al-Maslamani M. Tuberculosis of pancreas, the first case reported from Qatar. Int J Mycobacteriol. 2019;8(1):101-103.
2) Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. 2004;120(4):316-353.

Disclosures:
Duha Zaffar, MBBS, MD1, Chet Bahadur. Ranabhat, MBBS, MD2, Abdellatif Ismail, MBBS, MD2, Gurdeep Gogna, MD3, Gracia Viana. Rodriguez, MBBS, MD, DM4, Disha Sharma, MBBS5, Raymond Kim, MD, DM4. P2928 - Pancreatic Tuberculosis with Suspected Duodenal Fistula in an Immunocompromised Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Maryland Medical Center Midtown Campus, Baltimore, MD; 3American University of Antigua, Baltimore, MD; 4University of Maryland Medical Center, Baltimore, MD; 5University of Maryland, Baltimore, MD
Introduction: Pancreatic Tuberculosis (TB) is rare, likely due to the effect of pancreatic enzymes that confer protection against mycobacterium tuberculosis (MTB)¹·². However, suspicion should be high in those with pancreatic lesions and history of HIV, organ transplant or relevant immigration history. Our patient had pancreatic tuberculosis with suspected duodenal fistula with complete resolution of symptoms and the fistulous tract with a reduction of the size of the pancreatic lesion on imaging after 1 month of anti-tubercular therapy (ATT).
Case Description/Methods: A 38 years old male from Honduras presented with 3 days epigastric pain and hematochezia. He also reported fever, night sweats and abdominal pain for 2 months. Vitals signs showed blood pressure 86/52 mmHg, heart rate 119 beats/min, temperature 102.7 F. Oral thrush was noted on physical examination. Labs revealed hemoglobin 5.3 g/dL, positive HIV (CD4 count of 11 cells/uL), MTB positive blood culture. Diagnosis of disseminated TB was made and ATT was started. Computed Tomography (CT) abdomen showed multiple peripancreatic fluid collections with dependent air, suspicious of fistula with adjacent bowel (Figure 1). Upper endoscopy revealed a duodenal ulcer and suspected fistula (Figure 2) in the anterior duodenal sweep. Endoscopic ultrasound (EUS) with aspiration of pancreatic collections grew acid fast bacilli (Figure 3) consistent with pancreatic tuberculosis. In the interim, suspected fistula had completely healed and pancreatic collections had reduced in size. Interestingly, patient had completed more than one month of ATT by that time. As for the cause of duodenal ulcer, biopsies were negative for AFB, helicobacter pylori, cytomegalovirus, leishmaniasis and human herpes virus-8. There was no history of NSAID’s use but he had been smoking cigarettes for 26 years.
Discussion: Pancreatic lesions in a patient positive for MTB should warrant an early EUS with fine needle aspiration (FNA). This approach can confirm the diagnosis of a treatable condition, prevent unnecessary invasive procedures done to diagnose other similar presenting conditions such as pancreatic cancer and also help to avoid a surgical route for the management of bowel fistulas.
1) Ali M, Shaukat A, Al-Suwaidi Z, Al-Maslamani M. Tuberculosis of pancreas, the first case reported from Qatar. Int J Mycobacteriol. 2019;8(1):101-103.
2) Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. 2004;120(4):316-353.

Figure: (1) Peripancreatic fluid collections with dependent air, suspicious of fistula with adjacent bowel
(2) Suspected duodenal fistula in anterior duodenal sweep
(3) AFB found in pancreatic collections
(2) Suspected duodenal fistula in anterior duodenal sweep
(3) AFB found in pancreatic collections
Disclosures:
Duha Zaffar indicated no relevant financial relationships.
Chet Ranabhat indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Gurdeep Gogna indicated no relevant financial relationships.
Gracia Rodriguez indicated no relevant financial relationships.
Disha Sharma indicated no relevant financial relationships.
Raymond Kim: Apollo Endosurgery – Consultant. Cook medical – Consultant.
Duha Zaffar, MBBS, MD1, Chet Bahadur. Ranabhat, MBBS, MD2, Abdellatif Ismail, MBBS, MD2, Gurdeep Gogna, MD3, Gracia Viana. Rodriguez, MBBS, MD, DM4, Disha Sharma, MBBS5, Raymond Kim, MD, DM4. P2928 - Pancreatic Tuberculosis with Suspected Duodenal Fistula in an Immunocompromised Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

