Tuesday Poster Session
Category: Liver
P3928 - Healthcare Barriers for Liver Transplantation in an Immigrant with Cirrhosis From Transfusion-Acquired Hepatitis C & Secondary Iron Overload
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Lubaba Haque, DO
Kirk Kerkorian School of Medicine at UNLV
Las Vegas, NV
Presenting Author(s)
Lubaba Haque, DO1, Kyaw Min Tun, DO1, Rajan Amin, MD2, Shahid Wahid, MD3
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 2University of Nevada, Las Vegas, Las Vegas, NV; 3Valley Hospital Medical Center, Las Vegas, NV
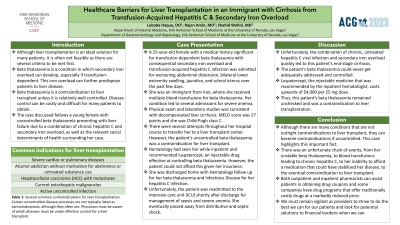
Introduction: Healthcare barriers are rampant throughout the United States, especially in socioeconomically disadvantaged and underserved communities, and underlie the need for patient advocacy. Liver transplantation is a long-awaited miracle with several relative contraindications, one of them being unaddressed health conditions. Uncontrolled beta thalassemia is one of them.
We discuss a woman with beta thalassemia with transfusion-acquired hepatitis C who is evaluated for decompensated cirrhosis and possible liver transplantation.
Case Description/Methods: This is a 25-year-old female with a history of transfusion-dependent beta thalassemia with secondary iron overload and transfusion-acquired hepatitis C presenting with abdominal distension, anasarca, and jaundice. The patient was a recent immigrant from Iran, where she had biweekly blood transfusions for beta thalassemia. She could not pursue treatment options back in Iran or in the U.S. given lack of insurance.
Laboratory studies revealed severe anemia, with a hemoglobin of 6.5 g/dL, and liver function derangements, with a total bilirubin of 8.3 mg/dL, and aminotransferases both at 80 IU/L. Abdominal ultrasound revealed diffuse hepatic disease with ascites. The patient’s Model for End-Stage Liver Disease (MELD) of 27 and Child-Pugh C score indicated an urgent need for liver transplantation. However, her untreated beta thalassemia was a contraindication. Unfortunately, she deteriorated in the intensive care unit (ICU) and expired.
Discussion: As a result of this patient’s immigrant status and lack of insurance, she was unable to afford a costly, but effective, drug for her thalassemia. Thus, she remained dependent on blood transfusions and died prior to being considered for liver transplant.
Healthcare costs are an enormous challenge. It is nearly impossible to get regular care in the U.S. without health insurance. One study revealed that even if one with public or no insurance gets on a waitlist for transplant, there is still a higher risk for waitlist mortality at about 43.8% total compared to those with private insurance at 12.3%. Resources that increase affordability, such as patient-assist programs, may be effective options with limitations. Seeing this issue on a more micro, state-level basis in coordination with local legislation, as well as on an individual basis to provide patient education on disease despite language barriers, may be beneficial in improving healthcare access for underprivileged patients.
Disclosures:
Lubaba Haque, DO1, Kyaw Min Tun, DO1, Rajan Amin, MD2, Shahid Wahid, MD3. P3928 - Healthcare Barriers for Liver Transplantation in an Immigrant with Cirrhosis From Transfusion-Acquired Hepatitis C & Secondary Iron Overload, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at UNLV, Las Vegas, NV; 2University of Nevada, Las Vegas, Las Vegas, NV; 3Valley Hospital Medical Center, Las Vegas, NV
Introduction: Healthcare barriers are rampant throughout the United States, especially in socioeconomically disadvantaged and underserved communities, and underlie the need for patient advocacy. Liver transplantation is a long-awaited miracle with several relative contraindications, one of them being unaddressed health conditions. Uncontrolled beta thalassemia is one of them.
We discuss a woman with beta thalassemia with transfusion-acquired hepatitis C who is evaluated for decompensated cirrhosis and possible liver transplantation.
Case Description/Methods: This is a 25-year-old female with a history of transfusion-dependent beta thalassemia with secondary iron overload and transfusion-acquired hepatitis C presenting with abdominal distension, anasarca, and jaundice. The patient was a recent immigrant from Iran, where she had biweekly blood transfusions for beta thalassemia. She could not pursue treatment options back in Iran or in the U.S. given lack of insurance.
Laboratory studies revealed severe anemia, with a hemoglobin of 6.5 g/dL, and liver function derangements, with a total bilirubin of 8.3 mg/dL, and aminotransferases both at 80 IU/L. Abdominal ultrasound revealed diffuse hepatic disease with ascites. The patient’s Model for End-Stage Liver Disease (MELD) of 27 and Child-Pugh C score indicated an urgent need for liver transplantation. However, her untreated beta thalassemia was a contraindication. Unfortunately, she deteriorated in the intensive care unit (ICU) and expired.
Discussion: As a result of this patient’s immigrant status and lack of insurance, she was unable to afford a costly, but effective, drug for her thalassemia. Thus, she remained dependent on blood transfusions and died prior to being considered for liver transplant.
Healthcare costs are an enormous challenge. It is nearly impossible to get regular care in the U.S. without health insurance. One study revealed that even if one with public or no insurance gets on a waitlist for transplant, there is still a higher risk for waitlist mortality at about 43.8% total compared to those with private insurance at 12.3%. Resources that increase affordability, such as patient-assist programs, may be effective options with limitations. Seeing this issue on a more micro, state-level basis in coordination with local legislation, as well as on an individual basis to provide patient education on disease despite language barriers, may be beneficial in improving healthcare access for underprivileged patients.
Disclosures:
Lubaba Haque indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Rajan Amin indicated no relevant financial relationships.
Shahid Wahid indicated no relevant financial relationships.
Lubaba Haque, DO1, Kyaw Min Tun, DO1, Rajan Amin, MD2, Shahid Wahid, MD3. P3928 - Healthcare Barriers for Liver Transplantation in an Immigrant with Cirrhosis From Transfusion-Acquired Hepatitis C & Secondary Iron Overload, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
