Tuesday Poster Session
Category: Biliary/Pancreas
P2929 - One Size Does Not Fit All: A Case of a PEG Tube Balloon Causing Biliary Obstruction and Pancreatitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Idrees Suliman, MD
Midwestern University
Mesa, AZ
Presenting Author(s)
Idrees Suliman, MD1, Oscar Lopez, MD2, Zachary M. Hanafi, DO3, Afsheen Moshtaghi, DO4, Mahomed Suliman, MD2
1Midwestern University, Mesa, AZ; 2El Centro Regional Medical Center, El Centro, CA; 3Verde Valley Medical Center, Cottonwood, AZ; 4Midwestern University, Cottonwood, AZ
Introduction: Perc Endoscopic Gast (PEG) feeding tubes are a common fixture in clinical practice. With routine care complications arising from PEG tube use are rare. Late complications associated with PEG tube placement include tube dysfunction, infection, peristomal leakage(PL), ulceration, and GOO. Should the external bolster be allowed to migrate away from the abdominal wall, the balloon can gain entrance to the duodenum. There have been 6 cases in the literature where migration of the balloon has caused obstructive pancreatitis. We present a similar case in a 91 year old female presenting with abdominal pain, nausea, and vomiting.
Case Description/Methods: A 91 yo female suffered a CVA 3 yrs ago resulting in oropharyngeal dysphagia, aphasia, LFT sided complete hemiparesis who required PEG tube placement. This is in a background sig for AFib, HTN, HLP, and cholecystectomy. Immediately following the stroke a 22Fr PEG tube was placed but was complicated by PL. In an effort to decrease leakage the feeding tube was gradually upsized to 26fr. This did not alleviate the problem so attempts were made to down size the PEG tube site. The tube was at 22F three months prior to hospital presentation. Two weeks prior to hospital presentation a 20fr tube was inserted.
She presented to the hospital with a two day history of nausea, vomiting, and grabbing of her abdomen appearing to be in pain. She was brought to a hospital for evaluation. PE was significant for the disc from the tube appearing to be lodged within the abdominal wall. This appeared to pull the abdomen from within with mild tension. Labs were significant for AST 503, ALT 433, Bili 1.7, Alk Phos 448, WBC 12.4, Lipase 1,455 (ULN 300). CT w/contrast showed a dilated CBD and PEG tube balloon located in duodenum. The balloon was deflated, retracted, reinflated and a larger disc was placed. This prevented distal migration of the PEG tube. She was also treated for acute pancreatitis with resumption of enteral feeding, intravenous fluids, and analgesia.
The next day there was improvement in her comfort and liver chemistries (Bili 0.8, ALT 291, AST 221, ALP 356). By the third day of admission her liver chemistries had normalized and she had returned to her baseline medical and functional status.
Discussion: This case highlights the observation that upsizing a PEG tube is not an adequate treatment strategy for PL. Additionally, careful monitoring of the feeding tube is required to prevent balloon migration. Balloon migration can result in obstructive pancreatitis.

Disclosures:
Idrees Suliman, MD1, Oscar Lopez, MD2, Zachary M. Hanafi, DO3, Afsheen Moshtaghi, DO4, Mahomed Suliman, MD2. P2929 - One Size Does Not Fit All: A Case of a PEG Tube Balloon Causing Biliary Obstruction and Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Midwestern University, Mesa, AZ; 2El Centro Regional Medical Center, El Centro, CA; 3Verde Valley Medical Center, Cottonwood, AZ; 4Midwestern University, Cottonwood, AZ
Introduction: Perc Endoscopic Gast (PEG) feeding tubes are a common fixture in clinical practice. With routine care complications arising from PEG tube use are rare. Late complications associated with PEG tube placement include tube dysfunction, infection, peristomal leakage(PL), ulceration, and GOO. Should the external bolster be allowed to migrate away from the abdominal wall, the balloon can gain entrance to the duodenum. There have been 6 cases in the literature where migration of the balloon has caused obstructive pancreatitis. We present a similar case in a 91 year old female presenting with abdominal pain, nausea, and vomiting.
Case Description/Methods: A 91 yo female suffered a CVA 3 yrs ago resulting in oropharyngeal dysphagia, aphasia, LFT sided complete hemiparesis who required PEG tube placement. This is in a background sig for AFib, HTN, HLP, and cholecystectomy. Immediately following the stroke a 22Fr PEG tube was placed but was complicated by PL. In an effort to decrease leakage the feeding tube was gradually upsized to 26fr. This did not alleviate the problem so attempts were made to down size the PEG tube site. The tube was at 22F three months prior to hospital presentation. Two weeks prior to hospital presentation a 20fr tube was inserted.
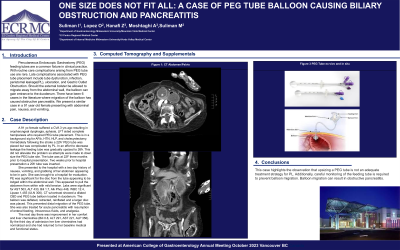
She presented to the hospital with a two day history of nausea, vomiting, and grabbing of her abdomen appearing to be in pain. She was brought to a hospital for evaluation. PE was significant for the disc from the tube appearing to be lodged within the abdominal wall. This appeared to pull the abdomen from within with mild tension. Labs were significant for AST 503, ALT 433, Bili 1.7, Alk Phos 448, WBC 12.4, Lipase 1,455 (ULN 300). CT w/contrast showed a dilated CBD and PEG tube balloon located in duodenum. The balloon was deflated, retracted, reinflated and a larger disc was placed. This prevented distal migration of the PEG tube. She was also treated for acute pancreatitis with resumption of enteral feeding, intravenous fluids, and analgesia.
The next day there was improvement in her comfort and liver chemistries (Bili 0.8, ALT 291, AST 221, ALP 356). By the third day of admission her liver chemistries had normalized and she had returned to her baseline medical and functional status.
Discussion: This case highlights the observation that upsizing a PEG tube is not an adequate treatment strategy for PL. Additionally, careful monitoring of the feeding tube is required to prevent balloon migration. Balloon migration can result in obstructive pancreatitis.

Figure: CT with contrast showing position of balloon in the duodenum
Disclosures:
Idrees Suliman indicated no relevant financial relationships.
Oscar Lopez indicated no relevant financial relationships.
Zachary Hanafi indicated no relevant financial relationships.
Afsheen Moshtaghi indicated no relevant financial relationships.
Mahomed Suliman indicated no relevant financial relationships.
Idrees Suliman, MD1, Oscar Lopez, MD2, Zachary M. Hanafi, DO3, Afsheen Moshtaghi, DO4, Mahomed Suliman, MD2. P2929 - One Size Does Not Fit All: A Case of a PEG Tube Balloon Causing Biliary Obstruction and Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
