Tuesday Poster Session
Category: Liver
P3936 - A Golden Spice With a Dark Side: A Case of Acute Liver Failure Due to Turmeric
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- HN
Haider Abbas A. Naqvi, MD
MedStar Health
Baltimore, MD
Presenting Author(s)
Fadi Alghzawi, MBBS, Christopher Haas, MD, PhD, Haider A. Naqvi, MD
MedStar Health, Baltimore, MD
Introduction: Herbal and dietary supplements have become increasingly popular in recent years, with at least half of the US population using some form of dietary supplementation. Turmeric is a popular supplement that has been demonstrated to be safe, and even hepatoprotective. Recently, however, there have been several reports of turmeric-induced liver injury.
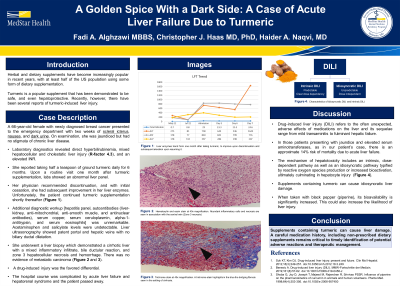
Case Description/Methods: A 66-year-old female with newly diagnosed breast cancer presented to the emergency department with two weeks of scleral icterus, nausea, and dark urine. On examination, she was jaundiced but had no stigmata of chronic liver disease. Laboratory diagnostics revealed direct hyperbilirubinemia, mixed hepatocellular and cholestatic liver injury (R-factor 4.3), and an elevated INR. She reported taking half a teaspoon of ground turmeric daily for 6 months. Upon a routine visit one month after turmeric supplementation, labs showed an abnormal liver panel. Her physician recommended discontinuation, and with initial cessation, she had subsequent improvement in her liver enzymes. Unfortunately, the patient continued turmeric supplementation shortly thereafter. Additional diagnostic workup was unremarkable. Liver ultrasonography showed patent portal and hepatic veins with no biliary ductal dilatation. She underwent a liver biopsy which demonstrated a cirrhotic liver with a mixed inflammatory infiltrate, bile ductular reaction, and zone 3 hepatocellular necrosis and hemorrhage. There was no evidence of metastatic carcinoma. A drug-induced injury was the favored differential. The hospital course was complicated by acute liver failure and hepatorenal syndrome and the patient passed away.
Discussion: Drug-induced liver injury refers to the often unexpected, adverse effects of medications on the liver and its sequelae range from mild transaminitis to fulminant hepatic failure. In those patients presenting with jaundice and elevated serum aminotransferases, as in our patient’s case, there is an approximate 14% risk of mortality due to acute liver failure. The mechanism of hepatotoxicity includes an intrinsic, dose-dependent pathway as well as an idiosyncratic pathway typified by reactive oxygen species production or increased bioactivation, ultimately culminating in hepatocyte injury. Supplements containing turmeric can cause idiosyncratic liver damage. When taken with black pepper (piperine), its bioavailability is significantly increased. This could also increase the likelihood of liver injury.

Disclosures:
Fadi Alghzawi, MBBS, Christopher Haas, MD, PhD, Haider A. Naqvi, MD. P3936 - A Golden Spice With a Dark Side: A Case of Acute Liver Failure Due to Turmeric, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
MedStar Health, Baltimore, MD
Introduction: Herbal and dietary supplements have become increasingly popular in recent years, with at least half of the US population using some form of dietary supplementation. Turmeric is a popular supplement that has been demonstrated to be safe, and even hepatoprotective. Recently, however, there have been several reports of turmeric-induced liver injury.
Case Description/Methods: A 66-year-old female with newly diagnosed breast cancer presented to the emergency department with two weeks of scleral icterus, nausea, and dark urine. On examination, she was jaundiced but had no stigmata of chronic liver disease. Laboratory diagnostics revealed direct hyperbilirubinemia, mixed hepatocellular and cholestatic liver injury (R-factor 4.3), and an elevated INR. She reported taking half a teaspoon of ground turmeric daily for 6 months. Upon a routine visit one month after turmeric supplementation, labs showed an abnormal liver panel. Her physician recommended discontinuation, and with initial cessation, she had subsequent improvement in her liver enzymes. Unfortunately, the patient continued turmeric supplementation shortly thereafter. Additional diagnostic workup was unremarkable. Liver ultrasonography showed patent portal and hepatic veins with no biliary ductal dilatation. She underwent a liver biopsy which demonstrated a cirrhotic liver with a mixed inflammatory infiltrate, bile ductular reaction, and zone 3 hepatocellular necrosis and hemorrhage. There was no evidence of metastatic carcinoma. A drug-induced injury was the favored differential. The hospital course was complicated by acute liver failure and hepatorenal syndrome and the patient passed away.
Discussion: Drug-induced liver injury refers to the often unexpected, adverse effects of medications on the liver and its sequelae range from mild transaminitis to fulminant hepatic failure. In those patients presenting with jaundice and elevated serum aminotransferases, as in our patient’s case, there is an approximate 14% risk of mortality due to acute liver failure. The mechanism of hepatotoxicity includes an intrinsic, dose-dependent pathway as well as an idiosyncratic pathway typified by reactive oxygen species production or increased bioactivation, ultimately culminating in hepatocyte injury. Supplements containing turmeric can cause idiosyncratic liver damage. When taken with black pepper (piperine), its bioavailability is significantly increased. This could also increase the likelihood of liver injury.

Figure: Top: Hematoxylin and eosin stain at 40x magnification. Abundant inflammatory cells and necrosis are seen in association with the central vein (Zone 3 necrosis). Bottom: Trichrome stain at 40x magnification. A trichrome stain highlights in the blue the bridging fibrosis seen in the setting of cirrhosis.
Disclosures:
Fadi Alghzawi indicated no relevant financial relationships.
Christopher Haas indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Fadi Alghzawi, MBBS, Christopher Haas, MD, PhD, Haider A. Naqvi, MD. P3936 - A Golden Spice With a Dark Side: A Case of Acute Liver Failure Due to Turmeric, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
