Tuesday Poster Session
Category: Biliary/Pancreas
P2938 - COVID-19-Associated Severe Necrotizing Hemorrhagic Pancreatitis – A Case Report
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Yamini Katamreddy, MD
West Anaheim Medical Center
Anaheim, California
Presenting Author(s)
Yamini Katamreddy, MD1, Snehamayi Ramayanam, MD1, Rewanth Katamreddy, MD2, Saikiran Mandyam, MD3, Olaniyi Fadeyi, MD1, Saisree Reddy Adla Jala, MD4, Asaad Hakim, MD1, Peyman Borghei, MD1
1West Anaheim Medical Center, Anaheim, CA; 2Saint Michael’s Medical Center, Newark, NJ; 3South East Health, Dothan, AL; 4Centinela Hospital Medical Center, Inglewood, CA
Introduction: Although a respiratory virus, COVID-19 can affect multiple organ systems, including hepatobiliary and gastrointestinal systems. Acute pancreatitis is commonly reported, with symptoms resolving in a few days. We report a case of acute necrotizing hemorrhagic pancreatitis caused by COVID-19 infection.
Case Description/Methods: A 65-year-old male with no past medical history presented with abdominal pain, generalized weakness, and syncope. On arrival, the patient was tachycardic with a blood pressure of 67/48 mm Hg. SARS antigen was positive for COVID-19. Hemoglobin on admission was 11.6 and lipase of 80. CT abdomen and pelvis with contrast showed acute pancreatitis with necrosis and retroperitoneal hemorrhage was suspected. CT angiography of the abdomen and pelvis showed active bleeding around the head of the pancreas. He has no history of alcohol or medication use, and no evidence of gallstones or hypertriglyceridemia. He was admitted to ICU for vasopressor support and broad-spectrum antibiotics were started. Repeat labs showed hemoglobin drop by more than 4 grams/dl. A massive transfusion protocol was initiated, and the patient received six units of packed red blood cells and 3-units of fresh frozen plasma (FFP). While undergoing transfusion, the patient had a cardiac arrest. After resuscitation, he underwent mesenteric angiography with embolization of multiple bleeding vessels. His prognosis was very and eventually succumbed.
Discussion: SARS CoV-2 affects vital organs in addition to the lung, including the heart, gastrointestinal tract, hepatobiliary tract, and kidney. Most common gastrointestinal presentations include nausea and vomiting, diarrhea, abdominal pain, liver enzyme abnormalities, and pancreatic injury [2,3]. The common causes of acute pancreatitis include gallstones and alcohol but rarely viral etiology [4]. COVID-19-induced pancreatic injury is caused by the virus's direct cytotoxic effect and a dysregulated immune response [2]. Because pancreatic cells express more ACE2 receptors, they are prime targets for dysregulated immune responses and subsequent pancreatitis [3,5]. COVID-19 infection complicated by acute necrotizing hemorrhagic pancreatitis is uncommon, with high morbidity and mortality, and there have been fewer than 5 cases reported. Treatment is mostly focused on surgical intervention, including debridement and necrosectomy in selected patients, besides fluids and empiric antibiotics. Surgery might not be feasible in hemodynamically unstable patients [5].

Disclosures:
Yamini Katamreddy, MD1, Snehamayi Ramayanam, MD1, Rewanth Katamreddy, MD2, Saikiran Mandyam, MD3, Olaniyi Fadeyi, MD1, Saisree Reddy Adla Jala, MD4, Asaad Hakim, MD1, Peyman Borghei, MD1. P2938 - COVID-19-Associated Severe Necrotizing Hemorrhagic Pancreatitis – A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1West Anaheim Medical Center, Anaheim, CA; 2Saint Michael’s Medical Center, Newark, NJ; 3South East Health, Dothan, AL; 4Centinela Hospital Medical Center, Inglewood, CA
Introduction: Although a respiratory virus, COVID-19 can affect multiple organ systems, including hepatobiliary and gastrointestinal systems. Acute pancreatitis is commonly reported, with symptoms resolving in a few days. We report a case of acute necrotizing hemorrhagic pancreatitis caused by COVID-19 infection.
Case Description/Methods: A 65-year-old male with no past medical history presented with abdominal pain, generalized weakness, and syncope. On arrival, the patient was tachycardic with a blood pressure of 67/48 mm Hg. SARS antigen was positive for COVID-19. Hemoglobin on admission was 11.6 and lipase of 80. CT abdomen and pelvis with contrast showed acute pancreatitis with necrosis and retroperitoneal hemorrhage was suspected. CT angiography of the abdomen and pelvis showed active bleeding around the head of the pancreas. He has no history of alcohol or medication use, and no evidence of gallstones or hypertriglyceridemia. He was admitted to ICU for vasopressor support and broad-spectrum antibiotics were started. Repeat labs showed hemoglobin drop by more than 4 grams/dl. A massive transfusion protocol was initiated, and the patient received six units of packed red blood cells and 3-units of fresh frozen plasma (FFP). While undergoing transfusion, the patient had a cardiac arrest. After resuscitation, he underwent mesenteric angiography with embolization of multiple bleeding vessels. His prognosis was very and eventually succumbed.
Discussion: SARS CoV-2 affects vital organs in addition to the lung, including the heart, gastrointestinal tract, hepatobiliary tract, and kidney. Most common gastrointestinal presentations include nausea and vomiting, diarrhea, abdominal pain, liver enzyme abnormalities, and pancreatic injury [2,3]. The common causes of acute pancreatitis include gallstones and alcohol but rarely viral etiology [4]. COVID-19-induced pancreatic injury is caused by the virus's direct cytotoxic effect and a dysregulated immune response [2]. Because pancreatic cells express more ACE2 receptors, they are prime targets for dysregulated immune responses and subsequent pancreatitis [3,5]. COVID-19 infection complicated by acute necrotizing hemorrhagic pancreatitis is uncommon, with high morbidity and mortality, and there have been fewer than 5 cases reported. Treatment is mostly focused on surgical intervention, including debridement and necrosectomy in selected patients, besides fluids and empiric antibiotics. Surgery might not be feasible in hemodynamically unstable patients [5].

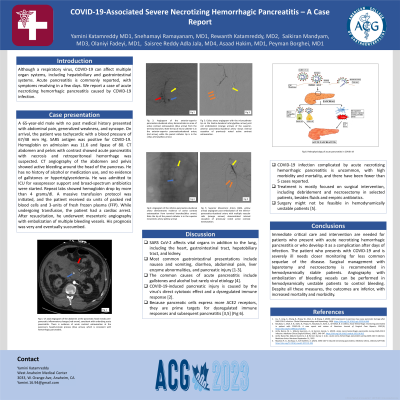
Figure: Fig 1: CT axial Angiogram of the abdomen at the pancreatic head reveals peri-pancreatic inflammatory changes (red arrow), consistent with underlying acute pancreatitis. There is evidence of acute contrast extravasation at the pancreas's head/uncinate process (blue arrow), which is consistent with hemorrhagic pancreatitis.
Fig 2: Angiogram of the anterior-superior pancreatico-duodenal artery demonstrates area of active contrast extravasation (blue arrow) from the terminal branches. Note the tip pf micro-catheter is in the anterior-superior pancreaticoduodenal artery (red arrow), while the parent catheter tip is in the celiac artery (yellow arrow)
Fig 3: Celiac artery angiogram with the microcatheter tip om the Gastro-duodenal artery (yellow arrow) post coil embolization (orange arrows) of the superior-anterior pancreatico-duodenal artery shows interval cessation of previously noted active contrast extravasation.
Fig 4: Angiogram of the inferior-pancreatico-duodenal artery demonstrates evidence of active contrast extravasation from terminal branches (blue arrow). Note the tip of the parent catheter is in the superior mesenteric artery (yellow arrow)
Fig 5: Superior Mesenteric Artery (SMA- yellow arrow) angiogram post embolization of the inferior-pancreatico-duodenal artery with multiple vascular coils (orange arrows) demonstrated interval cessation of previously noted active contrast extravasation.
Fig 6: Pathophysiology of acute pancreatitis in COVID-19
Fig 2: Angiogram of the anterior-superior pancreatico-duodenal artery demonstrates area of active contrast extravasation (blue arrow) from the terminal branches. Note the tip pf micro-catheter is in the anterior-superior pancreaticoduodenal artery (red arrow), while the parent catheter tip is in the celiac artery (yellow arrow)
Fig 3: Celiac artery angiogram with the microcatheter tip om the Gastro-duodenal artery (yellow arrow) post coil embolization (orange arrows) of the superior-anterior pancreatico-duodenal artery shows interval cessation of previously noted active contrast extravasation.
Fig 4: Angiogram of the inferior-pancreatico-duodenal artery demonstrates evidence of active contrast extravasation from terminal branches (blue arrow). Note the tip of the parent catheter is in the superior mesenteric artery (yellow arrow)
Fig 5: Superior Mesenteric Artery (SMA- yellow arrow) angiogram post embolization of the inferior-pancreatico-duodenal artery with multiple vascular coils (orange arrows) demonstrated interval cessation of previously noted active contrast extravasation.
Fig 6: Pathophysiology of acute pancreatitis in COVID-19
Disclosures:
Yamini Katamreddy indicated no relevant financial relationships.
Snehamayi Ramayanam indicated no relevant financial relationships.
Rewanth Katamreddy indicated no relevant financial relationships.
Saikiran Mandyam indicated no relevant financial relationships.
Olaniyi Fadeyi indicated no relevant financial relationships.
Saisree Reddy Adla Jala indicated no relevant financial relationships.
Asaad Hakim indicated no relevant financial relationships.
Peyman Borghei indicated no relevant financial relationships.
Yamini Katamreddy, MD1, Snehamayi Ramayanam, MD1, Rewanth Katamreddy, MD2, Saikiran Mandyam, MD3, Olaniyi Fadeyi, MD1, Saisree Reddy Adla Jala, MD4, Asaad Hakim, MD1, Peyman Borghei, MD1. P2938 - COVID-19-Associated Severe Necrotizing Hemorrhagic Pancreatitis – A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
