Tuesday Poster Session
Category: Biliary/Pancreas
P2939 - Now You See Me, Now You Don't: A Rare Case of Pembrolizumab Induced Vanishing Bile Duct Syndrome
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Bryant Pinto Javier, DO, MHA
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Bryant Pinto. Javier, DO, MHA1, Richi Kashyap, MD2, Uday Patel, DO1, Kumari Piryanka, MD1, Aimee League, MD3, Christopher Calcagno, DO1
1Parkview Medical Center, Pueblo, CO; 2North Alabama Medical Center, Florence, AL; 3Huntsville Hospital, Huntsville, AL
Introduction: Vanishing Bile Duct Syndrome (VBDS) is a disease involving bile duct injury and ductopenia progressing to liver failure. Typical presentation includes nausea, vomiting, fatigue, and elevated liver enzymes. Etiology is multifactorial, including autoimmune destruction. Histologically, periportal neutrophils, lymphocytes, eosinophils, cholangiocyte swelling, and ductular lymphocytic infiltration are seen in the acute phase. Progressive bile duct loss may result in liver failure and death.
Case Description/Methods: A 57-year-old African-American female initially presented for evaluation of left breast mass. She was diagnosed with stage IIB triple-negative breast cancer. Patient was started on Paclitaxel, Carboplatin, and Pembrolizumab combination. A week later, she was switched to Nab-paclitaxel due to an adverse reaction to taxol. Three weeks after, she developed worsening renal function: BUN 74, sCr 9.4. She had nausea, vomiting, and diarrhea and required hospitalization. After IV fluid resuscitation, her renal function declined, eventually requiring dialysis. Two weeks later, liver function tests: Bilirubin 8 mg/dl, AST 208 U/L, ALT 400 U/L, ALP 315 U/L. Prothrombin, albumin, and platelet count were normal. Chemotherapy was stopped due to immunotherapy-associated adverse effects. She clinically continued to worsen. Viral Hepatitis panel and autoimmune antibodies (ANA, SMA, AMA) were negative. No alcohol use was reported. She continued to develop edema progressing to anasarca with intractable nausea, vomiting, and encephalopathy. RUQ US showed borderline dilated 6 mm CBD. S/p cholecystectomy. No choledocholithiasis. Mild ascites. Coarse echotexture of the liver due to cirrhosis and hepatocellular disease. MRCP showed mildly dilated CBD with distal tapering in the ampulla. The liver biopsy showed significant ductopenia with minimal portal tract inflammation and no significant fibrosis, consistent with drug-related VBDS. After stopping chemotherapy, she underwent comfort measures and expired.
Discussion: There is limited data regarding the optimal treatment for VBDS. Treatment is supportive and focused on reducing symptoms associated with prolonged cholestasis. Though Pembrolizumab-induced VBDS has been rarely reported, close LFT monitoring, liver biopsy, and cessation of therapy are warranted if there is suspicion of VBDS. Some insight is provided by the Drug-Induced Liver Injury Network (DILIN) study. Early biopsy and cessation of therapy might play a role in improved outcomes.

Disclosures:
Bryant Pinto. Javier, DO, MHA1, Richi Kashyap, MD2, Uday Patel, DO1, Kumari Piryanka, MD1, Aimee League, MD3, Christopher Calcagno, DO1. P2939 - Now You See Me, Now You Don't: A Rare Case of Pembrolizumab Induced Vanishing Bile Duct Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Parkview Medical Center, Pueblo, CO; 2North Alabama Medical Center, Florence, AL; 3Huntsville Hospital, Huntsville, AL
Introduction: Vanishing Bile Duct Syndrome (VBDS) is a disease involving bile duct injury and ductopenia progressing to liver failure. Typical presentation includes nausea, vomiting, fatigue, and elevated liver enzymes. Etiology is multifactorial, including autoimmune destruction. Histologically, periportal neutrophils, lymphocytes, eosinophils, cholangiocyte swelling, and ductular lymphocytic infiltration are seen in the acute phase. Progressive bile duct loss may result in liver failure and death.
Case Description/Methods: A 57-year-old African-American female initially presented for evaluation of left breast mass. She was diagnosed with stage IIB triple-negative breast cancer. Patient was started on Paclitaxel, Carboplatin, and Pembrolizumab combination. A week later, she was switched to Nab-paclitaxel due to an adverse reaction to taxol. Three weeks after, she developed worsening renal function: BUN 74, sCr 9.4. She had nausea, vomiting, and diarrhea and required hospitalization. After IV fluid resuscitation, her renal function declined, eventually requiring dialysis. Two weeks later, liver function tests: Bilirubin 8 mg/dl, AST 208 U/L, ALT 400 U/L, ALP 315 U/L. Prothrombin, albumin, and platelet count were normal. Chemotherapy was stopped due to immunotherapy-associated adverse effects. She clinically continued to worsen. Viral Hepatitis panel and autoimmune antibodies (ANA, SMA, AMA) were negative. No alcohol use was reported. She continued to develop edema progressing to anasarca with intractable nausea, vomiting, and encephalopathy. RUQ US showed borderline dilated 6 mm CBD. S/p cholecystectomy. No choledocholithiasis. Mild ascites. Coarse echotexture of the liver due to cirrhosis and hepatocellular disease. MRCP showed mildly dilated CBD with distal tapering in the ampulla. The liver biopsy showed significant ductopenia with minimal portal tract inflammation and no significant fibrosis, consistent with drug-related VBDS. After stopping chemotherapy, she underwent comfort measures and expired.
Discussion: There is limited data regarding the optimal treatment for VBDS. Treatment is supportive and focused on reducing symptoms associated with prolonged cholestasis. Though Pembrolizumab-induced VBDS has been rarely reported, close LFT monitoring, liver biopsy, and cessation of therapy are warranted if there is suspicion of VBDS. Some insight is provided by the Drug-Induced Liver Injury Network (DILIN) study. Early biopsy and cessation of therapy might play a role in improved outcomes.

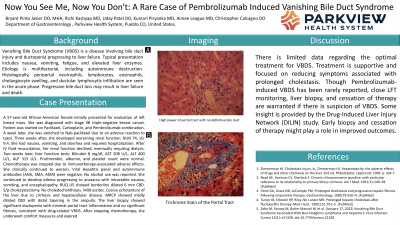
Figure: High power of portal tract with no definitive bile duct
Disclosures:
Bryant Javier indicated no relevant financial relationships.
Richi Kashyap indicated no relevant financial relationships.
Uday Patel indicated no relevant financial relationships.
Kumari Piryanka indicated no relevant financial relationships.
Aimee League indicated no relevant financial relationships.
Christopher Calcagno indicated no relevant financial relationships.
Bryant Pinto. Javier, DO, MHA1, Richi Kashyap, MD2, Uday Patel, DO1, Kumari Piryanka, MD1, Aimee League, MD3, Christopher Calcagno, DO1. P2939 - Now You See Me, Now You Don't: A Rare Case of Pembrolizumab Induced Vanishing Bile Duct Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
