Tuesday Poster Session
Category: Liver
P3941 - Hepatic Chylothorax in the Absence of Ascites: A Rare Pleural Effusion
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Adam Z. Koller, DO, MS
Palmetto General Hospital
Coral Gables, FL
Presenting Author(s)
Award: Presidential Poster Award
Adam Z. Koller, DO, MS1, Niraj Bhalani, DO2, Melissa Matheus, MD3, Karthik Mohan, DO2
1Palmetto General Hospital, Coral Gables, FL; 2Larkin Community Hospital, Miami, FL; 3Larkin Community Hospital, Palm Springs Campus, Doral, FL
Introduction: Cirrhosis accounts for only 1% of all chylothoraces and usually occurs in the presence of ascites. Hepatic chylothorax without ascites is extremely rare but important to recognize in order to effectively manage. We present a cirrhotic patient who developed a hepatic chylothorax in the absence of ascites.
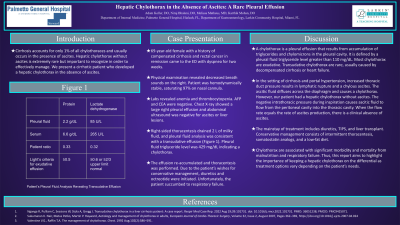
Case Description/Methods: 69-year-old female with a history of compensated cirrhosis and rectal cancer in remission came to the ED with dyspnea for two weeks. Physical examination revealed decreased breath sounds on the right. Patient was hemodynamically stable, saturating 97% on nasal cannula. Labs revealed anemia and thrombocytopenia. AFP and CEA were negative. Chest X-ray showed a large right pleural effusion and abdominal ultrasound was negative for ascites or liver lesions. Right-sided thoracentesis drained 2 L of milky fluid, and pleural fluid analysis was consistent with a transudative effusion (Figure 1). Pleural fluid triglyceride level was 429 mg/dL indicating a chylothorax. The next day, the effusion re-accumulated and thoracentesis was performed. Due to the patient’s wishes for conservative management, diuretics and octreotide were initiated. Unfortunately, the patient succumbed to respiratory failure.
Discussion: A chylothorax is a pleural effusion that results from accumulation of triglycerides and chylomicrons in the pleural cavity. It is defined by a pleural fluid triglyceride level greater than 110 mg/dL. Most chylothorax are exudative. Transudative chylothorax are rare, usually caused by decompensated cirrhosis or heart failure. In the setting of cirrhosis and portal hypertension, increased thoracic duct pressure results in lymphatic rupture and a chylous ascites. The ascitic fluid diffuses across the diaphragm and causes a chylothorax. However, our patient had a hepatic chylothorax without ascites. The negative intrathoracic pressure during inspiration causes ascitic fluid to flow from the peritoneal cavity into the thoracic cavity. When the flow rate equals the rate of ascites production, there is a clinical absence of ascites. The mainstay of treatment includes diuretics, TIPS, and liver transplant. Conservative management consists of intermittent thoracentesis, somatostatin analogs, and a low-fat diet. Chylothorax are associated with significant morbidity and mortality from malnutrition and respiratory failure. Thus, this report aims to highlight the importance of keeping a hepatic chylothorax on the differential as treatment options vary depending on the patient’s needs.
Disclosures:
Adam Z. Koller, DO, MS1, Niraj Bhalani, DO2, Melissa Matheus, MD3, Karthik Mohan, DO2. P3941 - Hepatic Chylothorax in the Absence of Ascites: A Rare Pleural Effusion, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Adam Z. Koller, DO, MS1, Niraj Bhalani, DO2, Melissa Matheus, MD3, Karthik Mohan, DO2
1Palmetto General Hospital, Coral Gables, FL; 2Larkin Community Hospital, Miami, FL; 3Larkin Community Hospital, Palm Springs Campus, Doral, FL
Introduction: Cirrhosis accounts for only 1% of all chylothoraces and usually occurs in the presence of ascites. Hepatic chylothorax without ascites is extremely rare but important to recognize in order to effectively manage. We present a cirrhotic patient who developed a hepatic chylothorax in the absence of ascites.
Case Description/Methods: 69-year-old female with a history of compensated cirrhosis and rectal cancer in remission came to the ED with dyspnea for two weeks. Physical examination revealed decreased breath sounds on the right. Patient was hemodynamically stable, saturating 97% on nasal cannula. Labs revealed anemia and thrombocytopenia. AFP and CEA were negative. Chest X-ray showed a large right pleural effusion and abdominal ultrasound was negative for ascites or liver lesions. Right-sided thoracentesis drained 2 L of milky fluid, and pleural fluid analysis was consistent with a transudative effusion (Figure 1). Pleural fluid triglyceride level was 429 mg/dL indicating a chylothorax. The next day, the effusion re-accumulated and thoracentesis was performed. Due to the patient’s wishes for conservative management, diuretics and octreotide were initiated. Unfortunately, the patient succumbed to respiratory failure.
Discussion: A chylothorax is a pleural effusion that results from accumulation of triglycerides and chylomicrons in the pleural cavity. It is defined by a pleural fluid triglyceride level greater than 110 mg/dL. Most chylothorax are exudative. Transudative chylothorax are rare, usually caused by decompensated cirrhosis or heart failure. In the setting of cirrhosis and portal hypertension, increased thoracic duct pressure results in lymphatic rupture and a chylous ascites. The ascitic fluid diffuses across the diaphragm and causes a chylothorax. However, our patient had a hepatic chylothorax without ascites. The negative intrathoracic pressure during inspiration causes ascitic fluid to flow from the peritoneal cavity into the thoracic cavity. When the flow rate equals the rate of ascites production, there is a clinical absence of ascites. The mainstay of treatment includes diuretics, TIPS, and liver transplant. Conservative management consists of intermittent thoracentesis, somatostatin analogs, and a low-fat diet. Chylothorax are associated with significant morbidity and mortality from malnutrition and respiratory failure. Thus, this report aims to highlight the importance of keeping a hepatic chylothorax on the differential as treatment options vary depending on the patient’s needs.
Disclosures:
Adam Koller indicated no relevant financial relationships.
Niraj Bhalani indicated no relevant financial relationships.
Melissa Matheus indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Adam Z. Koller, DO, MS1, Niraj Bhalani, DO2, Melissa Matheus, MD3, Karthik Mohan, DO2. P3941 - Hepatic Chylothorax in the Absence of Ascites: A Rare Pleural Effusion, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

