Tuesday Poster Session
Category: Biliary/Pancreas
P2942 - A Case Report: Ketamine-Induced Cholangiopathy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- NL
Naveena Luke, MD
Family Health Centers at NYU Langone
Presenting Author(s)
Naveena Luke, MD1, Navina Mohan, MD2, Jordan Axelrad, MD, MPH3
1Family Health Centers at NYU Langone, Brooklyn, NY; 2NYU Langone Hospital-Brooklyn, Brooklyn, NY; 3NYU Grossman School of Medicine, New York, NY
Introduction: Ketamine as a recreational hallucinogenic substance has grown increasingly popular and has sparse safety data regarding toxicity. There is also growing interest in its therapeutic efficacy for major depressive disorder, for which S-ketamine has been recently FDA-approved. Though ketamine use has been linked with urologic dysfunction, information is limited regarding its hepatotoxic and cholangiopathic effects. Here, we present a case of ketamine-induced cholangiopathy with severe obstructive uropathy.
Case Description/Methods: A previously healthy 23-year-old male presented to the hospital with fatigue, cachexia, and flank pain. He reported snorting ketamine twice daily for 6 months. Labs were significant for aspartate aminotransferase (AST) 516, alanine transaminase (ALT) 671, alkaline phosphatase (ALP) 1521, total bilirubin (TBili) 4.3, direct bilirubin (DBili) 3.5. The patient had a severe acute kidney injury (creatinine 5.56), hyperkalemia to 6.3, and hyponatremia to 108. His viral hepatitis panel was negative. Abdominal computerized tomography (CT) scan demonstrated severe bilateral hydroureteronephrosis and colonic distention secondary to renal obstruction. Abdominal ultrasound showed abnormal liver echotexture with linear hyperechoic tubular structures, and magnetic resonance cholangiopancreatography (MRCP) demonstrated fusiform dilatation of the common bile duct and intrahepatic biliary duct irregularity and no obstructing stone or lesion. After 30 days of abstinence from ketamine, liver function tests improved with AST 19, ALT 52, ALP 394, and Tbili and Dbili within normal limits.
Discussion: Ketamine is metabolized in the liver and excreted in bile and urine. The pathogenesis of ketamine-induced cholangiopathy has been hypothesized to be associated with direct hepatocyte damage as well as chronic smooth muscle stimulation around the bile ducts by the N-Methyl-D-aspartic acid receptor antagonist. This receptor activity may also precipitate cholangiopathy by dysregulating gallbladder motility. As seen here, findings and lab abnormalities typically resolve with cessation of ketamine use. In rare cases, however, there may be stricture formation requiring repeat MRCP and possible endoscopic retrograde cholangiopancreatography (ERCP).With ketamine’s success in mental health treatment, we can anticipate a surge of its use in the future; however, detailed toxicity data is imperative given the adverse effects in the hepatobiliary system.

Disclosures:
Naveena Luke, MD1, Navina Mohan, MD2, Jordan Axelrad, MD, MPH3. P2942 - A Case Report: Ketamine-Induced Cholangiopathy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Family Health Centers at NYU Langone, Brooklyn, NY; 2NYU Langone Hospital-Brooklyn, Brooklyn, NY; 3NYU Grossman School of Medicine, New York, NY
Introduction: Ketamine as a recreational hallucinogenic substance has grown increasingly popular and has sparse safety data regarding toxicity. There is also growing interest in its therapeutic efficacy for major depressive disorder, for which S-ketamine has been recently FDA-approved. Though ketamine use has been linked with urologic dysfunction, information is limited regarding its hepatotoxic and cholangiopathic effects. Here, we present a case of ketamine-induced cholangiopathy with severe obstructive uropathy.
Case Description/Methods: A previously healthy 23-year-old male presented to the hospital with fatigue, cachexia, and flank pain. He reported snorting ketamine twice daily for 6 months. Labs were significant for aspartate aminotransferase (AST) 516, alanine transaminase (ALT) 671, alkaline phosphatase (ALP) 1521, total bilirubin (TBili) 4.3, direct bilirubin (DBili) 3.5. The patient had a severe acute kidney injury (creatinine 5.56), hyperkalemia to 6.3, and hyponatremia to 108. His viral hepatitis panel was negative. Abdominal computerized tomography (CT) scan demonstrated severe bilateral hydroureteronephrosis and colonic distention secondary to renal obstruction. Abdominal ultrasound showed abnormal liver echotexture with linear hyperechoic tubular structures, and magnetic resonance cholangiopancreatography (MRCP) demonstrated fusiform dilatation of the common bile duct and intrahepatic biliary duct irregularity and no obstructing stone or lesion. After 30 days of abstinence from ketamine, liver function tests improved with AST 19, ALT 52, ALP 394, and Tbili and Dbili within normal limits.
Discussion: Ketamine is metabolized in the liver and excreted in bile and urine. The pathogenesis of ketamine-induced cholangiopathy has been hypothesized to be associated with direct hepatocyte damage as well as chronic smooth muscle stimulation around the bile ducts by the N-Methyl-D-aspartic acid receptor antagonist. This receptor activity may also precipitate cholangiopathy by dysregulating gallbladder motility. As seen here, findings and lab abnormalities typically resolve with cessation of ketamine use. In rare cases, however, there may be stricture formation requiring repeat MRCP and possible endoscopic retrograde cholangiopancreatography (ERCP).With ketamine’s success in mental health treatment, we can anticipate a surge of its use in the future; however, detailed toxicity data is imperative given the adverse effects in the hepatobiliary system.

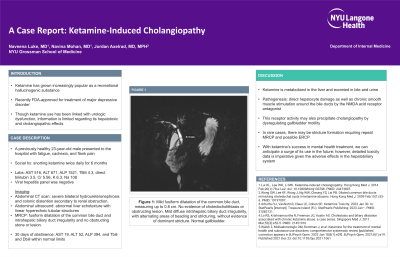
Figure: Mild fusiform dilatation of the common bile duct, measuring up to 0.8 cm. No evidence of choledocholithiasis or obstructing lesion. Mild diffuse intrahepatic biliary duct irregularity, with alternating areas of beading and stricturing, without evidence of dominant stricture. Normal gallbladder.
Disclosures:
Naveena Luke indicated no relevant financial relationships.
Navina Mohan indicated no relevant financial relationships.
Jordan Axelrad: AbbVie – received consulting fees. Adiso – received consulting fees. BioFire Diagnostics – Consultant, Grant/Research Support. Bristol Myers Squibb – received consulting fees. Fresenius Kabi – received consulting fees. Janssen – received consulting fees. Pfizer – received consulting fees.
Naveena Luke, MD1, Navina Mohan, MD2, Jordan Axelrad, MD, MPH3. P2942 - A Case Report: Ketamine-Induced Cholangiopathy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
