Tuesday Poster Session
Category: Liver
P3943 - Nephrogenic Ascites in a Patient With Multi-Organ Dysfunction: A Case Report and Discussion of Diagnostic Difficulties
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Michael Wright, BS
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Jay S. Shah, MD1, Michael Wright, BS1, John C. Tomkinson, MD2, Madeleine Hines Salge, MD1
1Baylor College of Medicine, Houston, TX; 2University of Tennessee Health Science Center, Memphis, TN
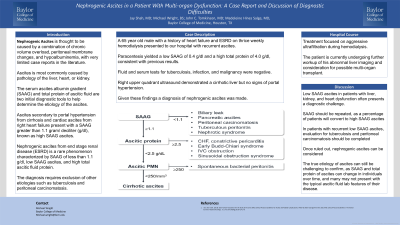
Introduction: Ascites is most commonly caused by pathology of the liver, heart, or kidney. The serum ascites albumin gradient (SAAG) and total protein of ascitic fluid are two initial diagnostic tools to help determine the etiology of the ascites. Ascites secondary to portal hypertension from cirrhosis and cardiac ascites from right heart failure present with a SAAG greater than 1.1 gram/ deciliter (g/dl), known as high SAAG ascites. Nephrogenic ascites from end stage renal disease (ESRD) is a rare phenomenon characterized by SAAG of less than 1.1 g/dl, low SAAG ascites, and high total ascitic fluid protein. The diagnosis requires exclusion of other etiologies such as tuberculosis and peritoneal carcinomatosis. Nephrogenic ascites is thought to be caused by a combination of chronic volume overload, peritoneal membrane changes, and hypoalbuminemia, with very limited case reports in the literature.
We discuss the case of a patient with liver, heart, and kidney dysfunction presenting with nephrogenic ascites in order to highlight this diagnostic difficulty.
Case Description/Methods: A 65 year old male with a history of heart failure and ESRD on thrice weekly hemodialysis presented to our hospital with recurrent ascites. Repeat paracentesis yielded a low SAAG of 0.4 g/dl and a high total protein of 4.0 g/dl, consistent with previous results. Fluid and serum tests for tuberculosis, infection, and malignancy were negative. Right upper quadrant ultrasound demonstrated a cirrhotic liver but no signs of portal hypertension. Given these findings, suspicion for cardiac, portal hypertension, tuberculosis, or malignancy associated ascites were diminished, and a diagnosis of nephrogenic ascites was made.
Treatment focused on aggressive ultrafiltration during hemodialysis. The patient is currently undergoing further workup of his abnormal liver imaging and consideration for possible multi-organ transplant.
Discussion: Low SAAG ascites in patients with liver, kidney, and heart dysfunction often presents a diagnostic challenge. SAAG should be repeated, as a percentage of patients will convert to high SAAG ascites. In patients with recurrent low SAAG ascites, evaluation for tuberculosis and peritoneal carcinomatosis should be completed. Once ruled out, nephrogenic ascites can be considered. The true etiology of ascites can still be challenging to confirm, as SAAG and total protein of ascites can change in individuals over time, and many may not present with the typical ascitic fluid lab features of their disease.
Disclosures:
Jay S. Shah, MD1, Michael Wright, BS1, John C. Tomkinson, MD2, Madeleine Hines Salge, MD1. P3943 - Nephrogenic Ascites in a Patient With Multi-Organ Dysfunction: A Case Report and Discussion of Diagnostic Difficulties, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Baylor College of Medicine, Houston, TX; 2University of Tennessee Health Science Center, Memphis, TN
Introduction: Ascites is most commonly caused by pathology of the liver, heart, or kidney. The serum ascites albumin gradient (SAAG) and total protein of ascitic fluid are two initial diagnostic tools to help determine the etiology of the ascites. Ascites secondary to portal hypertension from cirrhosis and cardiac ascites from right heart failure present with a SAAG greater than 1.1 gram/ deciliter (g/dl), known as high SAAG ascites. Nephrogenic ascites from end stage renal disease (ESRD) is a rare phenomenon characterized by SAAG of less than 1.1 g/dl, low SAAG ascites, and high total ascitic fluid protein. The diagnosis requires exclusion of other etiologies such as tuberculosis and peritoneal carcinomatosis. Nephrogenic ascites is thought to be caused by a combination of chronic volume overload, peritoneal membrane changes, and hypoalbuminemia, with very limited case reports in the literature.
We discuss the case of a patient with liver, heart, and kidney dysfunction presenting with nephrogenic ascites in order to highlight this diagnostic difficulty.
Case Description/Methods: A 65 year old male with a history of heart failure and ESRD on thrice weekly hemodialysis presented to our hospital with recurrent ascites. Repeat paracentesis yielded a low SAAG of 0.4 g/dl and a high total protein of 4.0 g/dl, consistent with previous results. Fluid and serum tests for tuberculosis, infection, and malignancy were negative. Right upper quadrant ultrasound demonstrated a cirrhotic liver but no signs of portal hypertension. Given these findings, suspicion for cardiac, portal hypertension, tuberculosis, or malignancy associated ascites were diminished, and a diagnosis of nephrogenic ascites was made.
Treatment focused on aggressive ultrafiltration during hemodialysis. The patient is currently undergoing further workup of his abnormal liver imaging and consideration for possible multi-organ transplant.
Discussion: Low SAAG ascites in patients with liver, kidney, and heart dysfunction often presents a diagnostic challenge. SAAG should be repeated, as a percentage of patients will convert to high SAAG ascites. In patients with recurrent low SAAG ascites, evaluation for tuberculosis and peritoneal carcinomatosis should be completed. Once ruled out, nephrogenic ascites can be considered. The true etiology of ascites can still be challenging to confirm, as SAAG and total protein of ascites can change in individuals over time, and many may not present with the typical ascitic fluid lab features of their disease.
Disclosures:
Jay Shah indicated no relevant financial relationships.
Michael Wright indicated no relevant financial relationships.
John Tomkinson indicated no relevant financial relationships.
Madeleine Hines Salge indicated no relevant financial relationships.
Jay S. Shah, MD1, Michael Wright, BS1, John C. Tomkinson, MD2, Madeleine Hines Salge, MD1. P3943 - Nephrogenic Ascites in a Patient With Multi-Organ Dysfunction: A Case Report and Discussion of Diagnostic Difficulties, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
