Tuesday Poster Session
Category: Liver
P3944 - Combined BRTO and ESG: A Multi-Disciplinary Approach to Recurrent NASH Allograft Fibrosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Jaclyn Tuck, MBBCh
Mayo Clinic College of Medicine
Scottsdale, AZ
Presenting Author(s)
Award: Presidential Poster Award
Jaclyn Tuck, MBBCh1, Rahul Pannala, MD2, Blanca Lizaola-Mayo, MD3, Justin M. Potter, MSN, ACNP-BC4, Marcela Salomao, MD2, Sadeer Alzubaidi, MD5, David M H. Chascsa, MD3
1Mayo Clinic College of Medicine, Scottsdale, AZ; 2Mayo Clinic, Scottsdale, AZ; 3Mayo Clinic, Phoenix, AZ; 4Mayo Clinic, Peoria, AZ; 5Mayo Clinic, Pheonix, AZ
Introduction: NASH can recur after liver transplant (LT) and lead to advanced liver fibrosis with portal hypertension (PH). PH is considered a relative contraindication to bariatric surgery due to risk of bleeding and hepatic decompensation. Minimally invasive therapies are needed to treat obesity in these patients. Endoscopic sleeve gastroplasty (ESG) is a safe and effective intervention for obesity but bleeding risk from PH still exists. As the fundus is usually intact in ESG, we proposed that in patients with isolated fundic varices in this setting, balloon-assisted retrograde trans-obliteration (BRTO) of gastric varices prior to ESG would allow for safe therapy with weight loss and improvement in NASH.
Case Description/Methods: A 54-year-old male who was 7 years post-LT for NASH cirrhosis exacerbated by alpha 1 antitrypsin presented with uncontrolled T2DM, elevated transaminases, BMI 33 kg/m2, and stage II CKD. Liver biopsy noted a rejection activity index 3/9, active steatohepatitis, NAFLD activity score (NAS) 6/8, macrosteatosis 35%, and F3 fibrosis. Endoscopy revealed isolated gastric varices (IGV1) without other features of PH. Supervised pharmacotherapy did not lead to sustained weight loss and surgery was considered contraindicated due to the finding of PH with IGV1 and concern for allograft cirrhosis. Targeted treatment of IGV1 was performed by BRTO of the mesenteric vein. After radiologic and endoscopic confirmation of variceal obliteration 4 weeks post BRTO, ESG was performed in a standard technique with sparing of the fundus. At 6 months post-ESG, the patient achieved 21% TBWL. Metabolic improvements included cessation of most DM medications, reduction in liver fibrosis F3-4 to F2-3 on imaging and liver biopsy. Substantial histologic improvement was also noted with steatohepatitis-S1, NAS 4/8, macrosteatosis 5%, F3 fibrosis and no rejection.
Discussion: Prior studies demonstrate that 30-35% of patients with NASH cirrhosis who undergo LT develop allograft steatohepatitis with 2% progressing to recurrent cirrhosis. Post-transplant PH is rare with 2.8% requiring intervention. There is limited data on gastric variceal management in allograft cirrhosis. One study found BRTO of gastric varices in transplant recipients had high success with few complications. Our case further highlights the utility of BRTO of isolated gastric varices in NASH allograft cirrhosis and that ESG can be performed safely and successfully to treat obesity, reduce NASH activity and potentially reverse advanced fibrosis.

Disclosures:
Jaclyn Tuck, MBBCh1, Rahul Pannala, MD2, Blanca Lizaola-Mayo, MD3, Justin M. Potter, MSN, ACNP-BC4, Marcela Salomao, MD2, Sadeer Alzubaidi, MD5, David M H. Chascsa, MD3. P3944 - Combined BRTO and ESG: A Multi-Disciplinary Approach to Recurrent NASH Allograft Fibrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Jaclyn Tuck, MBBCh1, Rahul Pannala, MD2, Blanca Lizaola-Mayo, MD3, Justin M. Potter, MSN, ACNP-BC4, Marcela Salomao, MD2, Sadeer Alzubaidi, MD5, David M H. Chascsa, MD3
1Mayo Clinic College of Medicine, Scottsdale, AZ; 2Mayo Clinic, Scottsdale, AZ; 3Mayo Clinic, Phoenix, AZ; 4Mayo Clinic, Peoria, AZ; 5Mayo Clinic, Pheonix, AZ
Introduction: NASH can recur after liver transplant (LT) and lead to advanced liver fibrosis with portal hypertension (PH). PH is considered a relative contraindication to bariatric surgery due to risk of bleeding and hepatic decompensation. Minimally invasive therapies are needed to treat obesity in these patients. Endoscopic sleeve gastroplasty (ESG) is a safe and effective intervention for obesity but bleeding risk from PH still exists. As the fundus is usually intact in ESG, we proposed that in patients with isolated fundic varices in this setting, balloon-assisted retrograde trans-obliteration (BRTO) of gastric varices prior to ESG would allow for safe therapy with weight loss and improvement in NASH.
Case Description/Methods: A 54-year-old male who was 7 years post-LT for NASH cirrhosis exacerbated by alpha 1 antitrypsin presented with uncontrolled T2DM, elevated transaminases, BMI 33 kg/m2, and stage II CKD. Liver biopsy noted a rejection activity index 3/9, active steatohepatitis, NAFLD activity score (NAS) 6/8, macrosteatosis 35%, and F3 fibrosis. Endoscopy revealed isolated gastric varices (IGV1) without other features of PH. Supervised pharmacotherapy did not lead to sustained weight loss and surgery was considered contraindicated due to the finding of PH with IGV1 and concern for allograft cirrhosis. Targeted treatment of IGV1 was performed by BRTO of the mesenteric vein. After radiologic and endoscopic confirmation of variceal obliteration 4 weeks post BRTO, ESG was performed in a standard technique with sparing of the fundus. At 6 months post-ESG, the patient achieved 21% TBWL. Metabolic improvements included cessation of most DM medications, reduction in liver fibrosis F3-4 to F2-3 on imaging and liver biopsy. Substantial histologic improvement was also noted with steatohepatitis-S1, NAS 4/8, macrosteatosis 5%, F3 fibrosis and no rejection.
Discussion: Prior studies demonstrate that 30-35% of patients with NASH cirrhosis who undergo LT develop allograft steatohepatitis with 2% progressing to recurrent cirrhosis. Post-transplant PH is rare with 2.8% requiring intervention. There is limited data on gastric variceal management in allograft cirrhosis. One study found BRTO of gastric varices in transplant recipients had high success with few complications. Our case further highlights the utility of BRTO of isolated gastric varices in NASH allograft cirrhosis and that ESG can be performed safely and successfully to treat obesity, reduce NASH activity and potentially reverse advanced fibrosis.

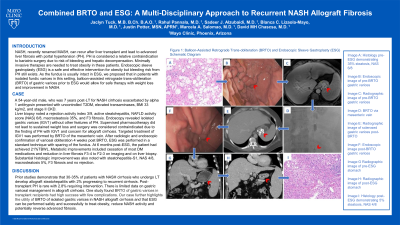
Figure: Figure 1: Balloon-Assisted Retrograde Trans-obliteration (BRTO) and Endoscopic Sleeve Gastroplasty (ESG) Schematic Diagram
Image A: Histology pre-ESG demonstrating 35% steatosis, NAS 6/8
Image B: Endoscopic image of Pre-BRTO gastric varices
Image C: Radiographic image of pre-BRTO gastric varices
Image D: BRTO via mesenteric vein
Image E: Radiographic image of sclerosed gastric varices post-BRTO
Image F: Endoscopic image post-BRTO gastric varices
Image G Radiographic image of pre-ESG stomach
Image H: Radiographic image of post-ESG stomach
Image I: Histology post-ESG demonstrating 5% steatosis, NAS 4/8
Image A: Histology pre-ESG demonstrating 35% steatosis, NAS 6/8
Image B: Endoscopic image of Pre-BRTO gastric varices
Image C: Radiographic image of pre-BRTO gastric varices
Image D: BRTO via mesenteric vein
Image E: Radiographic image of sclerosed gastric varices post-BRTO
Image F: Endoscopic image post-BRTO gastric varices
Image G Radiographic image of pre-ESG stomach
Image H: Radiographic image of post-ESG stomach
Image I: Histology post-ESG demonstrating 5% steatosis, NAS 4/8
Disclosures:
Jaclyn Tuck indicated no relevant financial relationships.
Rahul Pannala: Aimmune Therapeutics, a Nestlé Health Science company – Consultant. blue star genomics – Advisor or Review Panel Member. HCL technologies – Consultant.
Blanca Lizaola-Mayo indicated no relevant financial relationships.
Justin Potter indicated no relevant financial relationships.
Marcela Salomao indicated no relevant financial relationships.
Sadeer Alzubaidi indicated no relevant financial relationships.
David Chascsa indicated no relevant financial relationships.
Jaclyn Tuck, MBBCh1, Rahul Pannala, MD2, Blanca Lizaola-Mayo, MD3, Justin M. Potter, MSN, ACNP-BC4, Marcela Salomao, MD2, Sadeer Alzubaidi, MD5, David M H. Chascsa, MD3. P3944 - Combined BRTO and ESG: A Multi-Disciplinary Approach to Recurrent NASH Allograft Fibrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


