Tuesday Poster Session
Category: Liver
P3947 - Murine Typhus or Still's Disease? A Definitive Diagnosis From Liver Biopsy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Benjamin Heriford, DO
UT Health San Antonio
San Antonio, TX
Presenting Author(s)
Benjamin Heriford, DO1, Lily Kuo, MD2, Jonathan Selzman, DO3, Hamza Khan, MD1, Dakota Bigham, MD4, Umar Siddiqui, DO4, Katherine Willborn, MD5
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center San Antonio, San Antonio, TX; 3University of Texas Health Science Center at San Antonio, San Antonio, TX; 4University of Texas Health Science Center-San Antonio, San Antonio, TX; 5Audie Murphy VA Hospital, San Antonio, TX
Introduction: Murine typhus classically presents as a triad of fever, headache, and rash. We present a case of typhus masquerading as possible Still’s Disease.
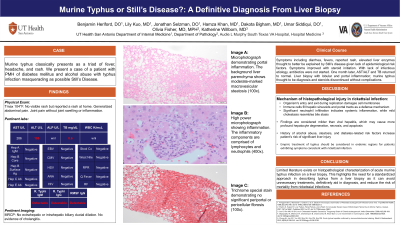
Case Description/Methods: A 38-year-old male with diabetes mellitus and alcohol abuse presented with persistent fever, reported rash, and arthralgia. Initial temperature was 104 Fahrenheit. He had normal white blood cell count, normal platelets, AST 286 U/L, ALT 186 U/L, and bilirubin 8.6 mg/dL. Imaging with CXR, KUB, Abdominal US, CT AP, and MRCP were nonrevealing. A hepatitis panel, autoimmune serologies, HIV and atypical pathogens for fever were also unremarkable. Given the persistent fever over hospital course plus elevated liver enzymes, he underwent a liver biopsy. Because work-up was overall unremarkable, he was placed on prednisone for possible Still’s Disease, and fever slowly improved with consequent hospital discharge. One month later, liver enzymes had returned to normal, and his liver biopsy revealed underlying steatosis with lobular and portal acute inflammation with centrilobular bile stasis due to Murine typhus, consistent with serologies. Still’s disease was excluded, and steroids subsequently discontinued.
Discussion: Histopathological findings of rickettsial infection can manifest in various ways. The mechanism involves the organism's entry and exit during replication, damaging cell membranes. Some studies report immune cells filling hepatic sinusoids and portal tracts as a defense mechanism. Another study reported significant neutrophil infiltration, indicative of systemic inflammation, while mild cholestasis resembling bile stasis was also observed in our case. One study even reported pseudo-granulomatous inflammation. These findings are considered generally more mild than viral hepatitis, which may cause more profound hepatocyte degeneration, necrosis, and apoptosis. Considering our patient's history of alcohol abuse and steatosis due to diabetes-related risk factors, he was at an increased risk of significant liver injury.
This case offers two important learning points. First, it contributes to the limited literature on histopathological characterization of acute murine typhus infection, highlighting the need for standardized approaches in describing typhus findings on liver biopsy. Second, empiric treatment of typhus should be considered in endemic regions for patients exhibiting symptoms consistent with rickettsial infection to prevent unnecessary interventions and reduce the risk of mortality.
Disclosures:
Benjamin Heriford, DO1, Lily Kuo, MD2, Jonathan Selzman, DO3, Hamza Khan, MD1, Dakota Bigham, MD4, Umar Siddiqui, DO4, Katherine Willborn, MD5. P3947 - Murine Typhus or Still's Disease? A Definitive Diagnosis From Liver Biopsy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center San Antonio, San Antonio, TX; 3University of Texas Health Science Center at San Antonio, San Antonio, TX; 4University of Texas Health Science Center-San Antonio, San Antonio, TX; 5Audie Murphy VA Hospital, San Antonio, TX
Introduction: Murine typhus classically presents as a triad of fever, headache, and rash. We present a case of typhus masquerading as possible Still’s Disease.
Case Description/Methods: A 38-year-old male with diabetes mellitus and alcohol abuse presented with persistent fever, reported rash, and arthralgia. Initial temperature was 104 Fahrenheit. He had normal white blood cell count, normal platelets, AST 286 U/L, ALT 186 U/L, and bilirubin 8.6 mg/dL. Imaging with CXR, KUB, Abdominal US, CT AP, and MRCP were nonrevealing. A hepatitis panel, autoimmune serologies, HIV and atypical pathogens for fever were also unremarkable. Given the persistent fever over hospital course plus elevated liver enzymes, he underwent a liver biopsy. Because work-up was overall unremarkable, he was placed on prednisone for possible Still’s Disease, and fever slowly improved with consequent hospital discharge. One month later, liver enzymes had returned to normal, and his liver biopsy revealed underlying steatosis with lobular and portal acute inflammation with centrilobular bile stasis due to Murine typhus, consistent with serologies. Still’s disease was excluded, and steroids subsequently discontinued.
Discussion: Histopathological findings of rickettsial infection can manifest in various ways. The mechanism involves the organism's entry and exit during replication, damaging cell membranes. Some studies report immune cells filling hepatic sinusoids and portal tracts as a defense mechanism. Another study reported significant neutrophil infiltration, indicative of systemic inflammation, while mild cholestasis resembling bile stasis was also observed in our case. One study even reported pseudo-granulomatous inflammation. These findings are considered generally more mild than viral hepatitis, which may cause more profound hepatocyte degeneration, necrosis, and apoptosis. Considering our patient's history of alcohol abuse and steatosis due to diabetes-related risk factors, he was at an increased risk of significant liver injury.
This case offers two important learning points. First, it contributes to the limited literature on histopathological characterization of acute murine typhus infection, highlighting the need for standardized approaches in describing typhus findings on liver biopsy. Second, empiric treatment of typhus should be considered in endemic regions for patients exhibiting symptoms consistent with rickettsial infection to prevent unnecessary interventions and reduce the risk of mortality.
Disclosures:
Benjamin Heriford indicated no relevant financial relationships.
Lily Kuo indicated no relevant financial relationships.
Jonathan Selzman indicated no relevant financial relationships.
Hamza Khan indicated no relevant financial relationships.
Dakota Bigham indicated no relevant financial relationships.
Umar Siddiqui indicated no relevant financial relationships.
Katherine Willborn indicated no relevant financial relationships.
Benjamin Heriford, DO1, Lily Kuo, MD2, Jonathan Selzman, DO3, Hamza Khan, MD1, Dakota Bigham, MD4, Umar Siddiqui, DO4, Katherine Willborn, MD5. P3947 - Murine Typhus or Still's Disease? A Definitive Diagnosis From Liver Biopsy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
