Tuesday Poster Session
Category: Liver
P3951 - Double Trouble: Simultaneous Encounter of Autoimmune Hepatitis and Chronic Hepatitis C Virus Infection
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- SS
Saher Sheikh, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Saher Sheikh, MD1, Jasmine Tsai, BS2, Sandra Gomez, MD1, Kevin Yeroushalmi, MD1, Jiten Desai, MD1, Rucha Jiyani, MD1, Kaleem Rizvon, MD1, Nausheer Khan, MD1, Paul Mustacchia, MD, MBA1, Krishnaiyer Subramani, MD1
1Nassau University Medical Center, East Meadow, NY; 2American University of the Caribbean School of Medicine, East Meadow, NY
Introduction: Autoimmune hepatitis (AIH) is a chronic inflammatory disease of the liver that can lead to cirrhosis and liver failure if left untreated. Chronic hepatitis C virus (HCV) infection is also a leading cause of chronic liver disease and can cause cirrhosis, hepatocellular carcinoma, and liver failure. Here we present a case of a patient with concurrent AIH and chronic HCV infection.
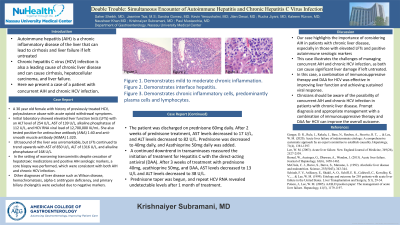
Case Description/Methods: 30 year old female with history of previously treated HCV, polysubstance abuse with acute opioid withdrawal symptoms. Initial laboratory showed elevated liver function tests (LFTs) with an ALT level of 254 U/L, AST of 139 U/L, alkaline phosphatase of 112 U/L, and HCV RNA viral load of 12,700,000 IU/mL. She also tested positive for antinuclear antibody (ANA) 1:40 and anti-smooth muscle antibody (ASMA) 1:320. Ultrasound of the liver was unremarkable, but LFTs continued to trend upwards with AST of 850 U/L, ALT of 1316 U/L, and alkaline phosphatase of 168 U/L. In the setting of worsening transaminitis despite cessation of hepatotoxic medications and positive AIH serologic markers, a core biopsy was performed, which were consistent with both AIH and chronic HCV infection. Other diagnoses of liver disease such as Wilson disease, hemochromatosis, alpha-1 antitrypsin deficiency, and primary biliary cholangitis were excluded due to negative markers. The patient was discharged on prednisone 60mg daily. After 2 weeks of prednisone treatment, AST levels decreased to 17 U/L, and ALT levels decreased to 82 U/L. Prednisone was decreased to 40mg daily, and Azathioprine 50mg daily was added. A continued downtrend in transaminases reassured the initiation of treatment for Hepatitis C with the direct-acting antiviral (DAA). After 3 weeks of treatment with prednisone 40mg, azathioprine 50mg, and DAA, AST levels decreased to 13 U/L and ALT levels decreased to 38 U/L. Prednisone taper was begun, and repeat HCV RNA revealed undetectable levels after 1 month of treatment.
Discussion: Our case highlights the importance of considering AIH in patients with chronic liver disease, especially in those with elevated LFTs and positive autoimmune serologic markers and illustrates the challenges of managing concurrent AIH and chronic HCV infection, as both can cause significant liver damage if left untreated. In this case, a combination of immunosuppressive therapy and DAA for HCV was effective in improving liver function and achieving sustained viral response.
Disclosures:
Saher Sheikh, MD1, Jasmine Tsai, BS2, Sandra Gomez, MD1, Kevin Yeroushalmi, MD1, Jiten Desai, MD1, Rucha Jiyani, MD1, Kaleem Rizvon, MD1, Nausheer Khan, MD1, Paul Mustacchia, MD, MBA1, Krishnaiyer Subramani, MD1. P3951 - Double Trouble: Simultaneous Encounter of Autoimmune Hepatitis and Chronic Hepatitis C Virus Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Nassau University Medical Center, East Meadow, NY; 2American University of the Caribbean School of Medicine, East Meadow, NY
Introduction: Autoimmune hepatitis (AIH) is a chronic inflammatory disease of the liver that can lead to cirrhosis and liver failure if left untreated. Chronic hepatitis C virus (HCV) infection is also a leading cause of chronic liver disease and can cause cirrhosis, hepatocellular carcinoma, and liver failure. Here we present a case of a patient with concurrent AIH and chronic HCV infection.
Case Description/Methods: 30 year old female with history of previously treated HCV, polysubstance abuse with acute opioid withdrawal symptoms. Initial laboratory showed elevated liver function tests (LFTs) with an ALT level of 254 U/L, AST of 139 U/L, alkaline phosphatase of 112 U/L, and HCV RNA viral load of 12,700,000 IU/mL. She also tested positive for antinuclear antibody (ANA) 1:40 and anti-smooth muscle antibody (ASMA) 1:320. Ultrasound of the liver was unremarkable, but LFTs continued to trend upwards with AST of 850 U/L, ALT of 1316 U/L, and alkaline phosphatase of 168 U/L. In the setting of worsening transaminitis despite cessation of hepatotoxic medications and positive AIH serologic markers, a core biopsy was performed, which were consistent with both AIH and chronic HCV infection. Other diagnoses of liver disease such as Wilson disease, hemochromatosis, alpha-1 antitrypsin deficiency, and primary biliary cholangitis were excluded due to negative markers. The patient was discharged on prednisone 60mg daily. After 2 weeks of prednisone treatment, AST levels decreased to 17 U/L, and ALT levels decreased to 82 U/L. Prednisone was decreased to 40mg daily, and Azathioprine 50mg daily was added. A continued downtrend in transaminases reassured the initiation of treatment for Hepatitis C with the direct-acting antiviral (DAA). After 3 weeks of treatment with prednisone 40mg, azathioprine 50mg, and DAA, AST levels decreased to 13 U/L and ALT levels decreased to 38 U/L. Prednisone taper was begun, and repeat HCV RNA revealed undetectable levels after 1 month of treatment.
Discussion: Our case highlights the importance of considering AIH in patients with chronic liver disease, especially in those with elevated LFTs and positive autoimmune serologic markers and illustrates the challenges of managing concurrent AIH and chronic HCV infection, as both can cause significant liver damage if left untreated. In this case, a combination of immunosuppressive therapy and DAA for HCV was effective in improving liver function and achieving sustained viral response.
Disclosures:
Saher Sheikh indicated no relevant financial relationships.
Jasmine Tsai indicated no relevant financial relationships.
Sandra Gomez indicated no relevant financial relationships.
Kevin Yeroushalmi indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Rucha Jiyani indicated no relevant financial relationships.
Kaleem Rizvon indicated no relevant financial relationships.
Nausheer Khan indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Krishnaiyer Subramani indicated no relevant financial relationships.
Saher Sheikh, MD1, Jasmine Tsai, BS2, Sandra Gomez, MD1, Kevin Yeroushalmi, MD1, Jiten Desai, MD1, Rucha Jiyani, MD1, Kaleem Rizvon, MD1, Nausheer Khan, MD1, Paul Mustacchia, MD, MBA1, Krishnaiyer Subramani, MD1. P3951 - Double Trouble: Simultaneous Encounter of Autoimmune Hepatitis and Chronic Hepatitis C Virus Infection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
