Tuesday Poster Session
Category: Liver
P3952 - Acute IRIS-Related HBV Flare Unmasked After Antiretroviral Therapy Initiation in a HIV/HBV Coinfected Patient
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Iqra Arshad, MD
Lincoln Medical Center
Saint Louis , MO
Presenting Author(s)
Iqra Arshad, MD, Mukti Gandhi, MD, Marcia Gossai, MD, Addi Feinstein, MD
Lincoln Medical Center, New York, NY
Introduction: 10-20% of HIV patients develop an exaggerated immune-mediated inflammatory response directed against opportunistic infections after antiretroviral therapy (ART) initiation, called Immune Reconstitution Inflammatory Syndrome (IRIS). HBV flares have been reported in 20-25% of patients within 2-8 weeks of starting ART among whom only 1-5% progress to clinical hepatitis.
Case Description/Methods: 24-year-old African American male who was diagnosed with HIV in 2018 and was on ART until his immigration to the United States when he lost follow up. He presented to our clinic to establish care. Baseline laboratory assessment showed HIV-load of 168,000 and CD4-count of 494. Patient was started on Bictegravir/Emtricitabine/Tenofovir alafenamide. Three weeks later, he presented to ED with complaints of polyarthralgia and loose stools and noted to have transaminases without hyperbilirubinemia (hepatocellular injury pattern) on repeated labs. Patient denied alcohol and herbal supplements use. Upon clinic follow up, an increasing trend of transaminases with evidence of cholestasis (mixed injury pattern) was noted and patient was admitted for closer monitoring. Work up revealed reactive HBsAg, HBeAg and HBcIgM with HBV-load 295,000. Other viral serologies, toxicology screen and autoimmune panel, all tested negative. Abdominal imaging was also unremarkable. ART was continued but switched to Rilpivirine/Tenofovir Alafenamide/Emtricitabine, considering the hypothetical risk of hepatotoxicity from Bictegravir/Emtricitabine/Tenofovir Alafenamide. Despite continuation of ART, transaminases were up trending, although patient remained asymptomatic. Patient was started on steroids for severe IRIS and diagnosis of acute IRIS-HBV flare was confirmed on Computerized tomography guided liver biopsy. Later, steroids were tapered off and ART was continued. Liver enzymes were normalized,HBV-load reduced significantly; HIV-load became undetectable and patient developed HBeAb (seroconversion) on subsequent follow ups. Patient is doing well and maintained on ART till date.
Discussion: Diagnostic criteria of IRIS-HBV Flare include worsening of liver enzymes after initiating ART, positive virological and immunological markers and absence of drug induced hepatotoxicity. Our patient met this criteria. Management usually involves continuation of ART targeting both viruses as discontinuation could worsen the flare and increase the risk of drug resistance with steroids reserve for severe cases only.

Disclosures:
Iqra Arshad, MD, Mukti Gandhi, MD, Marcia Gossai, MD, Addi Feinstein, MD. P3952 - Acute IRIS-Related HBV Flare Unmasked After Antiretroviral Therapy Initiation in a HIV/HBV Coinfected Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Lincoln Medical Center, New York, NY
Introduction: 10-20% of HIV patients develop an exaggerated immune-mediated inflammatory response directed against opportunistic infections after antiretroviral therapy (ART) initiation, called Immune Reconstitution Inflammatory Syndrome (IRIS). HBV flares have been reported in 20-25% of patients within 2-8 weeks of starting ART among whom only 1-5% progress to clinical hepatitis.
Case Description/Methods: 24-year-old African American male who was diagnosed with HIV in 2018 and was on ART until his immigration to the United States when he lost follow up. He presented to our clinic to establish care. Baseline laboratory assessment showed HIV-load of 168,000 and CD4-count of 494. Patient was started on Bictegravir/Emtricitabine/Tenofovir alafenamide. Three weeks later, he presented to ED with complaints of polyarthralgia and loose stools and noted to have transaminases without hyperbilirubinemia (hepatocellular injury pattern) on repeated labs. Patient denied alcohol and herbal supplements use. Upon clinic follow up, an increasing trend of transaminases with evidence of cholestasis (mixed injury pattern) was noted and patient was admitted for closer monitoring. Work up revealed reactive HBsAg, HBeAg and HBcIgM with HBV-load 295,000. Other viral serologies, toxicology screen and autoimmune panel, all tested negative. Abdominal imaging was also unremarkable. ART was continued but switched to Rilpivirine/Tenofovir Alafenamide/Emtricitabine, considering the hypothetical risk of hepatotoxicity from Bictegravir/Emtricitabine/Tenofovir Alafenamide. Despite continuation of ART, transaminases were up trending, although patient remained asymptomatic. Patient was started on steroids for severe IRIS and diagnosis of acute IRIS-HBV flare was confirmed on Computerized tomography guided liver biopsy. Later, steroids were tapered off and ART was continued. Liver enzymes were normalized,HBV-load reduced significantly; HIV-load became undetectable and patient developed HBeAb (seroconversion) on subsequent follow ups. Patient is doing well and maintained on ART till date.
Discussion: Diagnostic criteria of IRIS-HBV Flare include worsening of liver enzymes after initiating ART, positive virological and immunological markers and absence of drug induced hepatotoxicity. Our patient met this criteria. Management usually involves continuation of ART targeting both viruses as discontinuation could worsen the flare and increase the risk of drug resistance with steroids reserve for severe cases only.

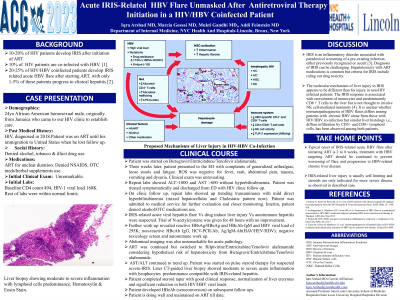
Figure: Liver biopsy showing acute inflammation with lymphocyte predominance (Hematoxylin & Eosin stain)
Disclosures:
Iqra Arshad indicated no relevant financial relationships.
Mukti Gandhi indicated no relevant financial relationships.
Marcia Gossai indicated no relevant financial relationships.
Addi Feinstein indicated no relevant financial relationships.
Iqra Arshad, MD, Mukti Gandhi, MD, Marcia Gossai, MD, Addi Feinstein, MD. P3952 - Acute IRIS-Related HBV Flare Unmasked After Antiretroviral Therapy Initiation in a HIV/HBV Coinfected Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
