Tuesday Poster Session
Category: Biliary/Pancreas
P2963 - The Pancreaticoduodenal Artery: An Unusual Culprit of Abdominal Pain
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

William Jones, MD
HCA Memorial Health University Medical Center
Savannah, GA
Presenting Author(s)
William Jones, MD1, Kathleen Humkey, MD1, Charles Duckworth, MD2
1HCA Memorial Health University Medical Center, Savannah, GA; 2Center for Digestive and Liver Health, Savannah, GA
Introduction: Pancreatic pseudocysts are a well known complication of pancreatitis. These lesions can be complicated by life-threatening bleeding and this should be considered as a differential in a patient presenting with abdominal pain, anemia, and a history of pancreatitis.
Case Description/Methods: A 38-year-old female with a past medical history of alcoholic cirrhosis, chronic pancreatitis with pseudocyst formation, ascites, and esophageal varices presented to the emergency department with complaints of epigastric abdominal pain and anemia. A CT scan of her abdomen and pelvis done in the ED showed an increase in the size of a previously described pseudocyst in the head of the pancreas from 4.7 x 4.1 cm to 5.1 x 4.5 cm when compared with an exam done 6 days prior with concern for active hemorrhage into the collection. Initial labs were notable for hemoglobin 7.6 g/dL, platelet count 118 K/uL, and INR 1.77. A follow up hemoglobin was 6.0 g/dL. A CT angiogram of the abdomen and pelvis showed active extravasation arising from the gastroduodenal artery branch into the pancreatic head/uncinate process. The patient was urgently taken to interventional radiology for embolization of the vessel. During arteriogram, she was found to have an abnormality of the pancreaticoduodenal artery which was likely eroded by the pseudocyst. The bleeding was controlled both proximally and distally via embolization with multiple coils. She was safely discharged home 4 days status post embolization.
Discussion: Pseudocyst formation is a possible sequelae of pancreatitis and can be complicated by infection, bleeding, obstruction, and rupture. Spontaneous hemorrhage within a pseudocyst has an incidence of less than 10%. Pseudocyst hemorrhage from the pancreaticoduodenal artery is one of the least common vessels (11%), more commonly occurring from the splenic artery (30-50%) and gastroduodenal artery (17%). [1] Unsurprisingly, pancreatic pseudocyst hemorrhage has been associated with high mortality rates. Management is endovascular transcatheter embolization or open surgical repair. [2] This case presents the need for clinicians to consider a pseudocyst hemorrhage when evaluating a patient with abdominal pain and decreasing hemoglobin.

Disclosures:
William Jones, MD1, Kathleen Humkey, MD1, Charles Duckworth, MD2. P2963 - The Pancreaticoduodenal Artery: An Unusual Culprit of Abdominal Pain, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1HCA Memorial Health University Medical Center, Savannah, GA; 2Center for Digestive and Liver Health, Savannah, GA
Introduction: Pancreatic pseudocysts are a well known complication of pancreatitis. These lesions can be complicated by life-threatening bleeding and this should be considered as a differential in a patient presenting with abdominal pain, anemia, and a history of pancreatitis.
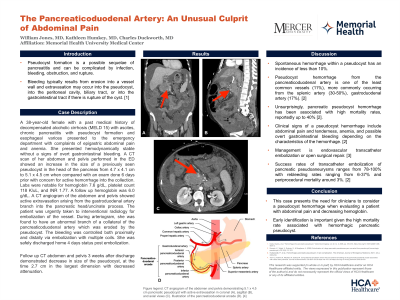
Case Description/Methods: A 38-year-old female with a past medical history of alcoholic cirrhosis, chronic pancreatitis with pseudocyst formation, ascites, and esophageal varices presented to the emergency department with complaints of epigastric abdominal pain and anemia. A CT scan of her abdomen and pelvis done in the ED showed an increase in the size of a previously described pseudocyst in the head of the pancreas from 4.7 x 4.1 cm to 5.1 x 4.5 cm when compared with an exam done 6 days prior with concern for active hemorrhage into the collection. Initial labs were notable for hemoglobin 7.6 g/dL, platelet count 118 K/uL, and INR 1.77. A follow up hemoglobin was 6.0 g/dL. A CT angiogram of the abdomen and pelvis showed active extravasation arising from the gastroduodenal artery branch into the pancreatic head/uncinate process. The patient was urgently taken to interventional radiology for embolization of the vessel. During arteriogram, she was found to have an abnormality of the pancreaticoduodenal artery which was likely eroded by the pseudocyst. The bleeding was controlled both proximally and distally via embolization with multiple coils. She was safely discharged home 4 days status post embolization.
Discussion: Pseudocyst formation is a possible sequelae of pancreatitis and can be complicated by infection, bleeding, obstruction, and rupture. Spontaneous hemorrhage within a pseudocyst has an incidence of less than 10%. Pseudocyst hemorrhage from the pancreaticoduodenal artery is one of the least common vessels (11%), more commonly occurring from the splenic artery (30-50%) and gastroduodenal artery (17%). [1] Unsurprisingly, pancreatic pseudocyst hemorrhage has been associated with high mortality rates. Management is endovascular transcatheter embolization or open surgical repair. [2] This case presents the need for clinicians to consider a pseudocyst hemorrhage when evaluating a patient with abdominal pain and decreasing hemoglobin.

Figure: Image 1. CT angiogram abdomen and pelvis axial image with 5.1 x 4.5 cm pancreatic pseudocyst (blue arrow) with active extravasation of contrast arising from a branch of the gastroduodenal artery (red arrow).
Disclosures:
William Jones indicated no relevant financial relationships.
Kathleen Humkey indicated no relevant financial relationships.
Charles Duckworth indicated no relevant financial relationships.
William Jones, MD1, Kathleen Humkey, MD1, Charles Duckworth, MD2. P2963 - The Pancreaticoduodenal Artery: An Unusual Culprit of Abdominal Pain, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
