Tuesday Poster Session
Category: Liver
P3963 - A Rare Case of Metastatic Inferior Vena Cava Leiomyosarcoma Presenting as a Primary Hepatic Malignancy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- PY
Patrick Yang, MD
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Patrick Yang, MD, Makeda Dawkins, MD, Aditi Desai, MBBS
Westchester Medical Center, Valhalla, NY
Introduction: Primary hepatic leiomyosarcomas (PHL) are rare malignant tumors originating from smooth muscle, accounting for 0.2-2% of hepatic malignancies. PHL is an aggressive cancer typically arising from intrahepatic vascular structures. Clinical presentation is often nonspecific, and patients may be asymptomatic despite advanced disease. Here, we report a rare case of inferior vena cava leiomyosarcoma presenting as a primary hepatic malignancy.
Case Description/Methods: A 56-year-old female presented with lower extremity edema, dyspnea on exertion, and fatigue. Her medical history included Hodgkin's Lymphoma treated with radiation, prior melanoma resection, and nonalcoholic fatty liver disease. Elevated D-dimer and pleural effusions on outpatient work-up prompted admission. CT abdomen revealed a 12.1cm heterogeneous, poorly defined, intrahepatic mass with compression and extension into the inferior vena cava (IVC), satellite lesions, omental infiltration, and a pulmonary nodule. Lab values including tumor markers AFP and CEA were normal. MRI abdomen showed a large, locally advanced liver malignancy with bilobar metastases and IVC invasion extending to the right heart. Thoracentesis for progressive hypoxia showed exudative effusion without malignant cells. Liver biopsy revealed leiomyosarcoma with high Ki-67 proliferation index. Immunohistochemistry was positive for smooth muscle actin and desmin, while negative for MART-1, S-100, SOX-10, Myogenin, AE1/AE3, and MyoD1, thus ruling out bile duct origin and supporting a diagnosis of metastatic IVC leiomyosarcoma. The patient was not a surgical candidate due to distal involvement and chemotherapy with Doxorubicin and Trebenectidin was initiated.
Discussion: PPHLs are aggressive and often diagnosed at an advanced stage. Clinical findings can be nonspecific with some remaining asymptomatic until tumor burden increases. Although there are reports linking PHL to Hodgkin's lymphoma, no established pathophysiologic association exists. Physicians should be vigilant in patients with a history of lymphoma and liver imaging abnormalities despite normal lab tests. Liver biopsy is crucial for diagnosis, revealing spindle-shaped cells with hyperchromatic nuclei and mitotic figures. Immunohistochemical analysis positive for SMA, desmin, and vimentin, and negative for cytokeratin, S100, AFP, CD34, CD117, further supports the diagnosis. Complete surgical resection offers the best chance of cure for localized disease, but treatment options for advanced cases remain limited.

Disclosures:
Patrick Yang, MD, Makeda Dawkins, MD, Aditi Desai, MBBS. P3963 - A Rare Case of Metastatic Inferior Vena Cava Leiomyosarcoma Presenting as a Primary Hepatic Malignancy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Primary hepatic leiomyosarcomas (PHL) are rare malignant tumors originating from smooth muscle, accounting for 0.2-2% of hepatic malignancies. PHL is an aggressive cancer typically arising from intrahepatic vascular structures. Clinical presentation is often nonspecific, and patients may be asymptomatic despite advanced disease. Here, we report a rare case of inferior vena cava leiomyosarcoma presenting as a primary hepatic malignancy.
Case Description/Methods: A 56-year-old female presented with lower extremity edema, dyspnea on exertion, and fatigue. Her medical history included Hodgkin's Lymphoma treated with radiation, prior melanoma resection, and nonalcoholic fatty liver disease. Elevated D-dimer and pleural effusions on outpatient work-up prompted admission. CT abdomen revealed a 12.1cm heterogeneous, poorly defined, intrahepatic mass with compression and extension into the inferior vena cava (IVC), satellite lesions, omental infiltration, and a pulmonary nodule. Lab values including tumor markers AFP and CEA were normal. MRI abdomen showed a large, locally advanced liver malignancy with bilobar metastases and IVC invasion extending to the right heart. Thoracentesis for progressive hypoxia showed exudative effusion without malignant cells. Liver biopsy revealed leiomyosarcoma with high Ki-67 proliferation index. Immunohistochemistry was positive for smooth muscle actin and desmin, while negative for MART-1, S-100, SOX-10, Myogenin, AE1/AE3, and MyoD1, thus ruling out bile duct origin and supporting a diagnosis of metastatic IVC leiomyosarcoma. The patient was not a surgical candidate due to distal involvement and chemotherapy with Doxorubicin and Trebenectidin was initiated.
Discussion: PPHLs are aggressive and often diagnosed at an advanced stage. Clinical findings can be nonspecific with some remaining asymptomatic until tumor burden increases. Although there are reports linking PHL to Hodgkin's lymphoma, no established pathophysiologic association exists. Physicians should be vigilant in patients with a history of lymphoma and liver imaging abnormalities despite normal lab tests. Liver biopsy is crucial for diagnosis, revealing spindle-shaped cells with hyperchromatic nuclei and mitotic figures. Immunohistochemical analysis positive for SMA, desmin, and vimentin, and negative for cytokeratin, S100, AFP, CD34, CD117, further supports the diagnosis. Complete surgical resection offers the best chance of cure for localized disease, but treatment options for advanced cases remain limited.

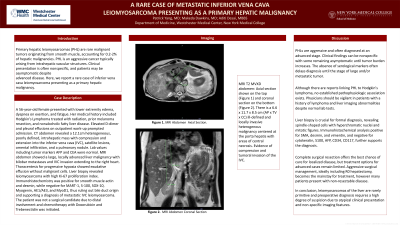
Figure: MRI T2 MVXD abdomen: Axial section shown on the left and coronal section on the right.
There is a 6.6 x 11.7 x 8.5 cm (AP x TV x CC) ill-defined and locally invasive heterogenous malignancy centered at the porta hepatis with areas of central necrosis. Compression and tumoral invasion of the IVC.
There is a 6.6 x 11.7 x 8.5 cm (AP x TV x CC) ill-defined and locally invasive heterogenous malignancy centered at the porta hepatis with areas of central necrosis. Compression and tumoral invasion of the IVC.
Disclosures:
Patrick Yang indicated no relevant financial relationships.
Makeda Dawkins indicated no relevant financial relationships.
Aditi Desai indicated no relevant financial relationships.
Patrick Yang, MD, Makeda Dawkins, MD, Aditi Desai, MBBS. P3963 - A Rare Case of Metastatic Inferior Vena Cava Leiomyosarcoma Presenting as a Primary Hepatic Malignancy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
