Tuesday Poster Session
Category: Liver
P3966 - Recovery from Acute Liver Failure After the Development of Cerebral Edema and Decerebrate Posturing
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Udita Gupta, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Udita Gupta, MD1, Derek Estes, MD1, Abhinav Vyas, MD2, Mohamed Shoreibah, MD1
1University of Alabama at Birmingham, Birmingham, AL; 2North Alabama Medical Center, Florence, AL
Introduction: Acute liver failure (ALF) is characterized by rapid onset encephalopathy and coagulopathy in patients without preexisting liver disease. ALF is a critical illness with an unfavorable prognosis, especially in patients who develop cerebral edema, and can result in potentially fatal uncal herniation. We report a patient who presented with ALF with Grade IV encephalopathy and decerebrate posturing who had a dramatic improvement with medical management.
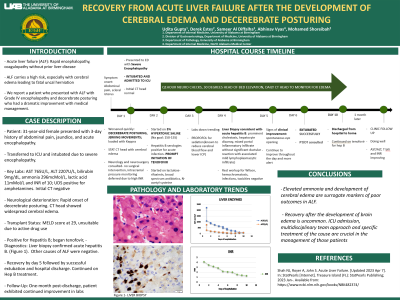
Case Description/Methods: A 31-year-old female with a history of substance use presented with abdominal pain and jaundice for 3 days. She was found to be profoundly encephalopathic requiring intubation and was transferred to our ICU. History did not reveal alcohol, OTC/herbal product use. Admission labs showed AST 765U/L, ALT 2207U/L, bilirubin 9mg/dL, ammonia 296mcMol/L, lactic acid 11mMol/L, and INR of 10. Urine drug screen was positive for amphetamines. Initial CT head was normal. Within a few hours, she started exhibiting decerebrate posturing. A stat CT head revealed diffuse cerebral edema. Neurology and neurosurgery were consulted. An exam performed without sedation revealed roving eye movements and intact brain stem reflexes. EEG showed diffuse suppression, suggesting severe cerebral dysfunction. MELD score was 29, but she was unsuitable for a liver transplant due to active drug use. Intracranial pressure monitoring was deferred. She was monitored with hourly neuro-checks, head of bed elevation, and propofol for sedation. She was started on 3% hypertonic saline for permissive hypernatremia. She had a positive HBsAg and HBcIgM and promptly started on tenofovir. She also received N-acetyl cysteine, lactulose, rifaximin, and antibiotics. Daily CT head to monitor cerebral edema remained stable. Her labs started improving. A liver biopsy revealed findings consistent with acute hepatitis B. Testing for other causes of ALF was negative. On day 5 the patient’s mental status began to improve, including spontaneous eye opening. She was successfully extubated on day 6. She was continued on tenofovir for Hepatitis B and discharged home on day 10. She followed up in clinic a month later and was found to be doing well with continued improvement in labs.
Discussion: Elevated ammonia and the development of cerebral edema are surrogate markers of poor outcomes in ALF. Recovery after the development of brain edema is uncommon. ICU admission, multidisciplinary team approach and specific treatment of the cause are crucial in the management of those patients.

Disclosures:
Udita Gupta, MD1, Derek Estes, MD1, Abhinav Vyas, MD2, Mohamed Shoreibah, MD1. P3966 - Recovery from Acute Liver Failure After the Development of Cerebral Edema and Decerebrate Posturing, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2North Alabama Medical Center, Florence, AL
Introduction: Acute liver failure (ALF) is characterized by rapid onset encephalopathy and coagulopathy in patients without preexisting liver disease. ALF is a critical illness with an unfavorable prognosis, especially in patients who develop cerebral edema, and can result in potentially fatal uncal herniation. We report a patient who presented with ALF with Grade IV encephalopathy and decerebrate posturing who had a dramatic improvement with medical management.
Case Description/Methods: A 31-year-old female with a history of substance use presented with abdominal pain and jaundice for 3 days. She was found to be profoundly encephalopathic requiring intubation and was transferred to our ICU. History did not reveal alcohol, OTC/herbal product use. Admission labs showed AST 765U/L, ALT 2207U/L, bilirubin 9mg/dL, ammonia 296mcMol/L, lactic acid 11mMol/L, and INR of 10. Urine drug screen was positive for amphetamines. Initial CT head was normal. Within a few hours, she started exhibiting decerebrate posturing. A stat CT head revealed diffuse cerebral edema. Neurology and neurosurgery were consulted. An exam performed without sedation revealed roving eye movements and intact brain stem reflexes. EEG showed diffuse suppression, suggesting severe cerebral dysfunction. MELD score was 29, but she was unsuitable for a liver transplant due to active drug use. Intracranial pressure monitoring was deferred. She was monitored with hourly neuro-checks, head of bed elevation, and propofol for sedation. She was started on 3% hypertonic saline for permissive hypernatremia. She had a positive HBsAg and HBcIgM and promptly started on tenofovir. She also received N-acetyl cysteine, lactulose, rifaximin, and antibiotics. Daily CT head to monitor cerebral edema remained stable. Her labs started improving. A liver biopsy revealed findings consistent with acute hepatitis B. Testing for other causes of ALF was negative. On day 5 the patient’s mental status began to improve, including spontaneous eye opening. She was successfully extubated on day 6. She was continued on tenofovir for Hepatitis B and discharged home on day 10. She followed up in clinic a month later and was found to be doing well with continued improvement in labs.
Discussion: Elevated ammonia and the development of cerebral edema are surrogate markers of poor outcomes in ALF. Recovery after the development of brain edema is uncommon. ICU admission, multidisciplinary team approach and specific treatment of the cause are crucial in the management of those patients.

Figure: Clinical Course
Disclosures:
Udita Gupta indicated no relevant financial relationships.
Derek Estes indicated no relevant financial relationships.
Abhinav Vyas indicated no relevant financial relationships.
Mohamed Shoreibah indicated no relevant financial relationships.
Udita Gupta, MD1, Derek Estes, MD1, Abhinav Vyas, MD2, Mohamed Shoreibah, MD1. P3966 - Recovery from Acute Liver Failure After the Development of Cerebral Edema and Decerebrate Posturing, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

